Impact of sarcopenia on intertrochanteric femoral fracture in the elderly
- Published
- Accepted
- Received
- Academic Editor
- Zhihua Han
- Subject Areas
- Orthopedics
- Keywords
- Femoral intertrochanteric fracture, Sarcopenia, Instrumental activities of daily living
- Copyright
- © 2022 Jiang et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2022. Impact of sarcopenia on intertrochanteric femoral fracture in the elderly. PeerJ 10:e13445 https://doi.org/10.7717/peerj.13445
Abstract
Objective
The aim of this study was to investigate the effect of skeletal sarcopenia on the prognosis of intertrochanteric fracture in the elderly.
Methods
We collected information on 144 patients with femoral intertrochanteric fracture (FIF). The influence of sarcopenia on the chance of death was determined using binary Probit regression analysis. For additional analysis, the Chow test was utilized to select the best distinguishing node in the instrumental activities of daily living (IADL) score. We looked for characteristics that were linked to a higher probability of death and a poor IADL outcome within 1 year. The data collected above were analyzed using logistic regression analysis. The internal calibration degree and model validity were assessed by GiViTI calibration.
Results
Sarcopenia, EuroQol-5D 1 month score, age, gender, and hypertension were identified as risk factors for death in older patients with FIF within a year by logistic regression analysis. Sarcopenia, psychotropics, BMI, and length of hospital stay were all found to be risk factors for poor IADL outcomes (P < 0.1). The calibration curves indicated that the anticipated and actual probabilities of these two models were very close. The study’s reliability coefficient was 0.671, showing a satisfactory level of reliability.
Conclusion
In elderly patients with FIF, sarcopenia, EuroQol-5D score, age, gender, and hypertension were risk factors for death; sarcopenia, hospital stay length, BMI were risk factors for poor quality of life.
Introduction
Intertrochanteric fracture is a fracture of the femoral neck from the base of the femur to just above the level of the lesser trochanter (Uzun, 2009; Butler et al., 2009). It is most common in the elderly. Fractures of the femoral trochanter often result in prolonged bed rest, which can lead to complications such as pneumonia and muscle atrophy, increasing the risk of death and reducing the quality of life in the elderly. Femoral intertrochanteric fracture (FIF) are usually treated surgically using rigid internal fixation (Uzun, 2009) and thereby avoiding a series of problems caused by prolonged bed rest (Weller et al., 2005). However, even with surgical treatment, the risk of postoperative death in these elderly patients is higher than in other elderly people. The prognosis of FIF elderly patients is affected by several factors (Peeters et al., 2016; Loggers et al., 2020).
Clinical observations have shown that elderly patients with FIF combined with sarcopenia often have a poor prognosis. The concept of sarcopenia was first introduced by Rosenberg in 1989 (Rosenberg, 1997). In 2010, the European Working Group on Sarcopenia in Older People (EWGSOP) defined sarcopenia as an age-related progressive reduction in whole-body skeletal muscle mass, strength, or physical function (Cruz-Jentoft et al., 2010). The examination of muscle mass is usually performed by bioelectrical impedance analysis (BIA), dual-energy x-ray absorptiometry (DXA), peripheral quantitative computed tomography (CT), and magnetic resonance imaging (MRI). Among them, BIA is widely used in clinical practice because of its low cost, safety, and convenience.
The incidence of sarcopenia increases with age (Cruz-Jentoft et al., 2019). Sarcopenia can seriously affect mobility in older adults. The prognosis for elderly patients with FIF in combination with sarcopenia is often poor (Landi et al., 2017; Yoo et al., 2018). However, there is no satisfactory way to predict mortality and quality of life after the surgery for femoral trochanteric fracture. The aim of this study was to investigate the effect of skeletal sarcopenia on the prognosis of intertrochanteric fracture in the elderly. Using a combination of clinical observations and literature review, we conducted a study suggesting that sarcopenia and several other factors affect mortality and quality of life in patients with FIF 1 year after surgery.
Materials and Methods
Population
We collected information on 144 patients with intertrochanteric fracture of the femur who attended the Department of Orthopedics, Langfang People’s Hospital from June 2016 to June 2020 in this cross-sectional study. We obtained patient data through the electronic medical records of patients aged >65 years and patients without cognitive impairment or language impairment and other conditions that might make it impossible for them to understand the questionnaire and complete follow-up information. The exclusion criteria were as follows: patients with major diseases or decompensation of vital organs, patients with bilateral fractures and other surgeries on the same side or malignancies and life-threatening conditions that occurred during the follow-up period, and patient data that the investigator determined were not credible. All included patients underwent standard treatments. All participants were informed of the study orally and in writing, and written informed consent was also obtained. The ethical procedures of the study procedures were in accordance with the Declaration of Helsinki. The study was supported by Langfang People’s Hospital Ethics Committee (IRB approval number 2016003). The clinical characteristics of each patient were collected, including age, sex, marital status, education, survival, body mass index, residential status, income, depression, sensory impairment, diabetes, hypertension, American Society of Anesthesiologists EuroQol-5D questionnaire score, presence of osteoporosis, instrumental activities of daily living score, and history of anti-osteoporosis medication use. Surveys were completed at admission and follow up (1, 6, and 12 months). All survey data were entered by two researchers and checked for accuracy.
Diagnosis of sarcopenia
Bioelectrical impedance analysis (BIA) is an effective method for diagnosing sarcopenia (Wang et al., 2016; Chen et al., 2020). The appendicular skeletal muscle mass (ASM) of the extremities was measured by the BIA method using a body composition analyzer (TANITA-MC180) immediately after the patients were admitted with fractures, and muscle strength was assessed by ASM/H2. To complete the BIA measurement, the subjects held the electrode in their hand, with the body was resting on the hospital bed, and the foot was placed on the foot electrode. With the assistance of medical personnel, the patient completed the test in under a minute. This study adopted the Asian Working Group on Sarcopenia risk screening method and EWGSOP2 to define sarcopenia (Chen et al., 2014; Cruz-Jentoft et al., 2019). Therefore, muscle mass ≤7.0 kg/m2 in men and ≤6.0 kg/m2 in women was used as a diagnostic criterion for sarcopenia.
EuroQol-5D questionnaire
The EuroQol-5D is a questionnaire that is widely used as a clinical and an economic assessment tool for the health-related quality of life (EuroQol Group, 1990). Each dimension of the EuroQol-5D scoring system is divided into three levels. Instrumental activities of daily living scores are completed using the Lawton and Brody scale (Lawton & Brody, 1969). These eight scoring items followed previous studies. Previous researched included these items included in the scale assessed were as previous research (Alekna et al., 2018).
Statistical analysis
Statistical analysis was performed using SPSS version 22 software (IBM Corp., Armonk, NY, USA) and R software (version 3.5.3; R Core Team, 2019). The measurement data were expressed as mean plus/minus standard deviation and statistically analysed by an independent sample t-test; count data were expressed as percentages (%) and statistically analysed by the χ2 test; the non-parametric rank sum test was used for the grade information. Reliability analysis was used to study the reliability of the collected data (Eisinga, Grotenhuis & Pelzer, 2013). A Cronbach’s α coefficient higher than 0.6 indicates acceptable reliability and <0.6 indicates poor reliability. To analyze the effect of sarcopenia on the risk of death in older patients with FIF, we performed a binary Probit regression analysis using sarcopenia as the independent variable and death as the dependent variable. As described in previous studies, the Chow test was used to determine the best distinguishing node of the IADL score, by SAS9.3 software, allowing it to be further analyzed (Liang et al., 2017). A 10-fold cross-validation method using recursive feature elimination (RFE) with random forest as classifier and R-packet insertion was used to screen features associated with risk of death and adverse IADL outcomes within 1 year in patients with age-related FIF (Wang et al., 2020). Eventually, 144 samples were included in the analysis, and logistic regression analysis was performed with the characteristics obtained above as in previous studies (Kang et al., 2020; Zhou et al., 2021; Ying et al., 2021). To assess the internal calibration degree and the validity of the model, the givitiR package of the R software was used to plot the GiViTI calibration bands of this logistic model (Gebremariam et al., 2021). In this study, P < 0.05 was considered significant.
Results
Demographic characteristics of patients
Among the 144 participants, 35 patients (24.3%) had comorbid sarcopenia on admission, and there were 36 males and 108 females. The demographics of the participants are shown in Table 1. Body mass index (BMI), death, income, availability of chaperones, history of hip fracture, EuroQol-5D 1-month score, EuroQol-5D 6-month score, EuroQol-5D 12-month score, IADL 1-month score, IADL 6-month score, and IADL-12 month score were important risk factors for sarcopenia. The reliability coefficient value of the study is 0.671, which is greater than 0.6, indicating the acceptable quality of the study data for reliability (Table S1). Table 2 shows the binary Probit regression analysis that was performed with sarcopenia as the independent variable and death as the dependent variable, using the model equation Probit (P) = −2.210 + 0.822 × Sarcopenia (where p represents the risk of death within 1 year in patients with FIF). The results suggest that sarcopenia is a risk factor for poor prognosis in older patients with FIF. The marginal effect value was 0.162, which suggests that sarcopenia increases the mortality risk by 16.19% in older patients with FIF in short-term follow up.
| Items | Sarcopenia (n = 144) | Total (n = 144) | P-value | ||
|---|---|---|---|---|---|
| NO (n = 109) | YES (n = 35) | ||||
| Age | 84.40 ± 6.38 | 86.29 ± 6.96 | 84.86 ± 6.55 | 0.14 | |
| BMI | 26.24 ± 3.98 | 24.34 ± 3.00 | 25.78 ± 3.85 | 0.011* | |
| Death | No | 100 (91.74) | 25 (71.43) | 125 (86.81) | 0.002** |
| Yes | 9 (8.26) | 10 (28.57) | 19 (13.19) | ||
| Intervention | No | 54 (49.54) | 23 (65.71) | 77 (53.47) | 0.095 |
| Yes | 55 (50.46) | 12 (34.29) | 67 (46.53) | ||
| Gender | Female | 82 (75.23) | 26 (74.29) | 108 (75.00) | 0.911 |
| Man | 27 (24.77) | 9 (25.71) | 36 (25.00) | ||
| Illiteracy | No | 74 (67.89) | 21 (60.00) | 95 (65.97) | 0.391 |
| Yes | 35 (32.11) | 14 (40.00) | 49 (34.03) | ||
| Marital status | Married | 35 (32.11) | 11 (31.43) | 46 (31.94) | 0.94 |
| Single | 74 (67.89) | 24 (68.57) | 98 (68.06) | ||
| Availability of chaperones | Yes | 19 (17.43) | 12 (34.29) | 31 (21.53) | 0.035* |
| No | 90 (82.57) | 23 (65.71) | 113 (78.47) | ||
| Income (yuan) | <500 | 1 (0.92) | 4 (11.43) | 5 (3.47) | 0.020* |
| 500–1,000 | 92 (84.40) | 24 (68.57) | 116 (80.56) | ||
| 1,000–1,500 | 13 (11.93) | 6 (17.14) | 19 (13.19) | ||
| >=1,500 | 3 (2.75) | 1 (2.86) | 4 (2.78) | ||
| Intervention complications | No | 92 (84.40) | 30 (85.71) | 122 (84.72) | 0.851 |
| Yes | 17 (15.60) | 5 (14.29) | 22 (15.28) | ||
| Hypertension | No | 25 (22.94) | 9 (25.71) | 34 (23.61) | 0.736 |
| Yes | 84 (77.06) | 26 (74.29) | 110 (76.39) | ||
| Diabetes | No | 71 (65.14) | 27 (77.14) | 98 (68.06) | 0.185 |
| Yes | 38 (34.86) | 8 (22.86) | 46 (31.94) | ||
| Dyslipidemia | No | 73 (66.97) | 26 (74.29) | 99 (68.75) | 0.417 |
| Yes | 36 (33.03) | 9 (25.71) | 45 (31.25) | ||
| Osteoporosis | No | 101 (92.66) | 32 (91.43) | 133 (92.36) | 0.811 |
| Yes | 8 (7.34) | 3 (8.57) | 11 (7.64) | ||
| Previous hip fracture history | No | 106 (97.25) | 29 (82.86) | 135 (93.75) | 0.004** |
| Yes | 3 (2.75) | 6 (17.14) | 9 (6.25) | ||
| Psychotropics | No | 58 (53.21) | 20 (57.14) | 78 (54.17) | 0.685 |
| Yes | 51 (46.79) | 15 (42.86) | 66 (45.83) | ||
| Bisphosphontes | No | 106 (97.25) | 35 (100.00) | 141 (97.92) | 0.321 |
| Yes | 3 (2.75) | 0 (0.00) | 3 (2.08) | ||
| Sensory disturbances | No | 52 (47.71) | 16 (45.71) | 68 (47.22) | 0.837 |
| Yes | 57 (52.29) | 19 (54.29) | 76 (52.78) | ||
| ASA score | I | 1 (0.92) | 0 (0.00) | 1 (0.69) | 0.945 |
| II | 35 (32.11) | 11 (31.43) | 46 (31.94) | ||
| III | 65 (59.63) | 21 (60.00) | 86 (59.72) | ||
| IV | 8 (7.34) | 3 (8.57) | 11 (7.64) | ||
| Depressive mood | No | 49 (44.95) | 14 (40.00) | 63 (43.75) | 0.607 |
| Yes | 60 (55.05) | 21 (60.00) | 81 (56.25) | ||
| EuroQol-5D 1-month score | 53.30 ± 17.24 | 43.20 ± 16.64 | 51.28 ± 17.53 | 0.009** | |
| EuroQol-5D 6-month score | 59.20 ± 19.32 | 49.60 ± 22.36 | 57.28 ± 20.24 | 0.033* | |
| EuroQol-5D 12-month score | 60.20 ± 19.38 | 46.00 ± 19.84 | 57.36 ± 20.22 | 0.001** | |
| IADL 1-month score | 2.25 ± 1.40 | 1.36 ± 0.81 | 2.07 ± 1.35 | P < 0.001** | |
| IADL 6-month score | 2.21 ± 1.74 | 1.64 ± 1.44 | 2.1 ± 1.7 | 0.134 | |
| IADL 12-month score | 2.29 ± 1.88 | 1.32 ± 0.85 | 2.1 ± 1.77 | P < 0.001** | |
| Items | Regression coefficient | standard error | Z value | P value | 95% CI | Marginal effects |
|---|---|---|---|---|---|---|
| Sarcopenia | 0.822 | 0.284 | 2.898 | 0.004 | [0.266–1.378] | 0.162 |
| Intercept | −2.21 | 0.413 | −5.354 | P < 0.001 | [−3.019 to −1.401] | – |
Notes:
Dependent variable: Death.
McFadden R: 0.074.
Cox & Snell R: 0.056.
Nagelkerke R: 0.104.
Determination of the optimal IADL node and screening of key prognostic features
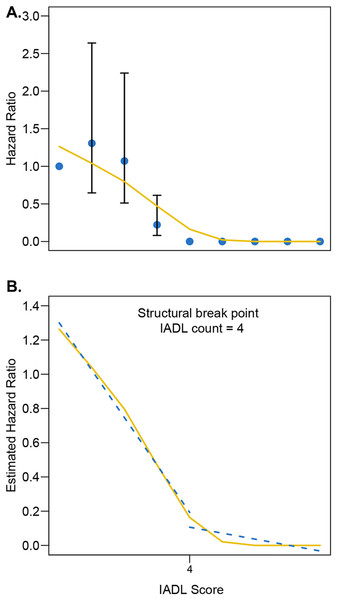
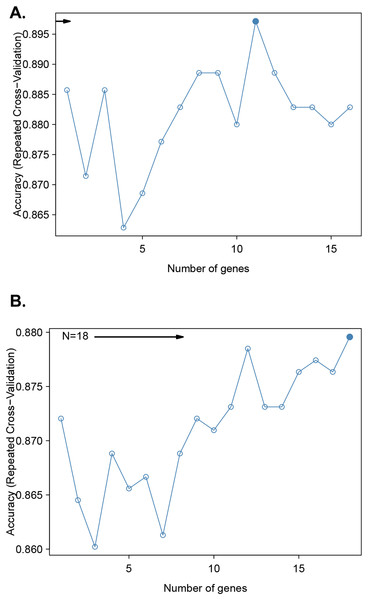
After adjusting for sex, age, sarcopenia, and intervention modality, the Chow test was used to determine the best distinguishing node for the IADL score after femoral trochanter fracture in patients (Fig. 1A). An IADL score of four was considered to give the best discrimination. A recursive feature elimination algorithm based on the random forest model was used to analyze the relationship between the predictive accuracy and the number of selected features (Fig. 1B). The highest accuracy in predicting the mortality risk within 1 year in older patients with FIF was achieved by including 11 factors: EuroQol-5D 1-month score, EuroQol-5D 6-month score, EuroQol-5D 12-month score, age, sex, hypertension, psychotropics, intervention, marital status, sarcopenia, and depressive mood history (Fig. 2A). The highest accuracy in predicting IADL outcome in older patients with FIF was achieved by including 18 factors (Fig. 2B). The excessive number of parameters makes clinical work difficult, so we have selected the 11 most relevant ones here to improve clinical usability (including hospital stay duration, sarcopenia, age, illiteracy, depressive mood, BMI, dyslipidemia, psychotropics, diabetes, availability of chaperones, and intervention).
Figure 1: (A–B) The Chow test was used to establish the best differentiating node for the IADL score after accounting for sex, age, sarcopenia, and intervention mode.
The Chow test was used to establish the best differentiating node for the IADL score after accounting for sex, age, sarcopenia, and intervention mode.Figure 2: A recursive feature elimination algorithm was used to investigate the relationship between predictive accuracy and the number of selected features.
Predictive accuracy for mortality risk within 1 year in older femoral intertrochanteric fracture patients (A) and predictive accuracy for poor IADL outcome (B).Muscular sarcopenia is associated with mortality and reduced quality of life within 1 year after FIF in older patients
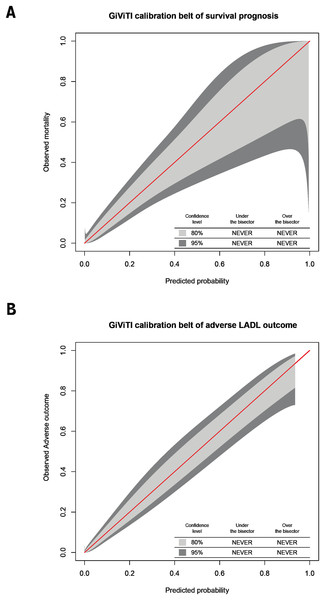
The variables screened from the random forest model were included in the unconditional binary logistic regression analysis, which showed that the EuroQol-5D 1-month score, age, sex, hypertension, and sarcopenia were risk factors for death within 1 year in elderly patients with FIF (P < 0.1; Table 3). Hospital stay duration, sarcopenia, BMI, and psychotropics were risk factors for adverse IADL outcomes in patients with FIF (P < 0.1; Table 4). The calibration curves of the logistic regression models for the risk of death within 1 year and adverse IADL outcome in older patients with FIF suggested a strong agreement between the predicted and actual probabilities of these two models (Figs. 3A and 3B). In conclusion, sarcopenia is a common risk factor for adverse IADL outcomes and death within 1 year in older patients with FIF.
| Variable | Prediction model | ||
|---|---|---|---|
| β | Odds ratio (95% CI) | P-value | |
| (Intercept) | −2.279 | 0.102 [0–95.853] | 0.514 |
| EuroQol-5D 1-month score | 0.058 | 1.06 [1.017–1.104] | 0.006 |
| EuroQol-5D 6-month score | 0.046 | 1.047 [0.977–1.121] | 0.191 |
| EuroQol-5D 12-month score | 0.038 | 1.039 [0.971–1.111] | 0.267 |
| Age | −0.089 | 0.915 [0.842–0.993] | 0.033 |
| Gender | −1.475 | 0.229 [0.076–0.692] | 0.009 |
| Hypertension | −1.056 | 0.348 [0.134–0.902] | 0.030 |
| Psychotropics | −0.367 | 0.693 [0.279–1.721] | 0.429 |
| Intervention | 0.251 | 1.285 [0.535–3.085] | 0.574 |
| Marital status | −0.574 | 0.563 [0.205–1.549] | 0.266 |
| Sarcopenia | −1.990 | 0.137 [0.015–1.225] | 0.075 |
| Depressive mood history | 0.334 | 1.396 [0.49–3.981] | 0.533 |
Note:
β is the regression coefficient.
| Variable | Prediction model | |||
|---|---|---|---|---|
| β | Odds ratio (95% CI) | P-value | ||
| (Intercept) | −7.200 | 0 [0–6.87] | 0.122 | |
| Hospital stay time | 0.290 | 1.34 [1.08–1.67] | 0.008 | |
| Sarcopenia | 1.450 | 4.25 [1.22–14.77] | 0.023 | |
| Age | 0.010 | 1.01 [0.92–1.1] | 0.861 | |
| Illiteracy | 0.580 | 1.79 [0.54–5.99] | 0.344 | |
| Depressive mood | −0.460 | 0.63 [0.2–1.99] | 0.434 | |
| BMI | 0.140 | 1.15 [0.98–1.35] | 0.088 | |
| Dyslipidemia | −1.000 | 0.37 [0.08–1.76] | 0.211 | |
| Psychotropics | −1.270 | 0.28 [0.07–1.07] | 0.063 | |
| Diabetes | −0.910 | 0.4 [0.09–1.85] | 0.243 | |
| Availability of chaperones | −1.120 | 0.33 [0.08–1.28] | 0.108 | |
| Intervention | −0.870 | 0.42 [0.12–1.54] | 0.190 | |
Note:
BMI, Body Mass Index; β is the regression coefficient.
Figure 3: Calibration plots.
In older individuals with femoral intertrochanteric fracture, calibration plots of logistic regression models for 1-year mortality risk (A) and unfavorable IADL outcome (B).Discussion
This study confirms that sarcopenia is a common risk factor for death and decreased quality of life among elderly patients with FIF and is the greatest risk factor for increased mortality and decreased quality of life.
Sarcopenia was diagnosed by BIA, and the quality of life of patients was quantified using EuroQol-5D and IADL scores. A binary Probit regression analysis with sarcopenia as the independent variable and death as the dependent variable yielded the model equation Probit (P) = −2.210 + 0.822* sarcopenia (where p represents the risk of death within 1 year in patients with FIF). This condition indicated that sarcopenia is a risk factor for death within 1 year among elderly patients with FIF and increases the risk by 16.19%. The unconditional binary logistic regression analysis revealed that the five risk factors (P < 0.1) for death within 1 year among elderly patients with FIF were EuroQol-5D 1 month score, age, sex, hypertension and sarcopenia, and the four risk factors (P < 0.1) for adverse IADL outcome among elderly patients with FIF were the length of hospital stay, sarcopenia, BMI and psychotropics. Therefore, sarcopenia is a common risk factor for death and decreased quality of life postoperatively within 1 year among elderly patients with FIF.
EuroQol-5D is a critical metric for determining a patient’s quality of life. In this study, patients without concomitant sarcopenia after intertrochanteric fracture had a EuroQol-5D 1 month score of 0.53, a EuroQol-5D 6 month score of 0.59, and a EuroQol-5D 12 month score of 0.60. Patients’ EuroQol-5D scores were greater than in a previous fracture injury study (Vu et al., 2019a). This could be a result of China’s rapid development in medical care in recent years, which, along with effective preoperative and postoperative care, has resulted in patients having better overall EuroQol-5D scores. Patients without concomitant sarcopenia had EuroQol-5D scores that were similar to fragile elderly patients in a previous study (EuroQol-5D = 0.58) (Vu et al., 2019b). Patients with sarcopenia had a EuroQol-5D 1-month score of 0.43, a EuroQol-5D 6-month score of 0.49, and a 12-month EuroQol-5D score of 0.46, which was similar to the earlier study of the elderly after a fall injury (Vu et al., 2019b). Sarcopenia appears to be a risk factor for femur intertrochanteric fractures. Furthermore, EuroQol-5D was lower in patients after a greater intertrochanteric fracture of the femur than after dengue fever (EuroQol-5D = 0.66), respiratory diseases (EuroQol-5D = 0.66), skin diseases (EuroQol-5D = 0.73), human immunodeficiency virus (HIV) (EuroQol-5D = 0.8), diabetes (EuroQol-5D = 0.8), and the general population under COVID-19 (EuroQol-5D = 0.95) (Tran et al., 2018b, 2018a, 2020; Nguyen et al., 2018, 2019). We found that the EuroQol-5D 1-month score was a significant risk factor for 1-year mortality.
The Kaplan–Meier estimate found that sarcopenia did not affect the 1-year mortality (P = 0.793) but significantly affected the 5-year mortality (P = 0.028) (Kim et al., 2018). Yoo et al. (2018) compared the effects of both sarcopenia and osteoporosis among elderly patients with hip fracture, accounting for 7.8% in general, 10.3% in combination with sarcopenia, 15.1% in combination with both sarcopenia and osteoporosis, and 5.1% in patients with osteoporosis only (Yoo et al., 2018). Unlike other studies that included osteoporosis as an influencing factor for mortality, our study revealed that osteoporosis alone did not increase mortality among elderly patients with hip fracture, and mortality was significantly higher in patients with concomitant sarcopenia and osteoporosis. Previous studies have also concluded that sarcopenia is not associated with postoperative mortality among elderly patients with FIF (Di Monaco et al., 2015; González-Montalvo et al., 2016; Chang et al., 2018).
Unlike previous studies, our study compared the effects of sarcopenia on the 1-year mortality among elderly patients with FIF in China, showing that 28.57% of patients with skeletal sarcopenia and osteoporosis died within 1 years, which was much higher than the 8.26% in those with FIF alone. Not only was sarcopenia confirmed as a significant risk factor for increased 1-year mortality and reduced quality of life among elderly patients with FIF, but also four other risk factors for higher 1-year mortality (EuroQol-5D 1-month score, age, sex and hypertension) and three risk factors for reduced quality of life (length of hospital stay, BMI and use of psychotropics) were identified. This finding provides information on additional interventions to reduce mortality and improve the quality of life of elderly patients with FIF.
Femoral intertrochanter fractures are known as the last fracture in life and are of concern because of their high post-fracture mortality and serious impact on quality of life. This study further confirms that sarcopenia is an important risk factor for mortality or reduced quality of life after a FIF among elderly patients, and sarcopenia can be prevented or improved by increasing the nutritional intake and exercise training; therefore, the following factors should be considered: (1) pay attention to the muscle quality of the elderly individuals to prevent sarcopenia and (2) screen elderly patients with sarcopenia among those with FIF to detect and intervene in sarcopenia promptly to reduce improve quality of life and mortality among elderly patients with FIF. Generally, the muscle mass is assessed with dual-energy X-ray imaging, BIA, CT or MRI (Heymsfield et al., 2015). Among them, CT or MRI measures the cross-sectional area of the skeletal muscle of the body to calculate the skeletal muscle index (SMI) for a more accurate diagnosis of sarcopenia (Nemec et al., 2017). However, CT exposes the patients to a higher radiation dose, and MRI is expensive and takes a long time to carry out; therefore, we used BIA to diagnose sarcopenia, which may overestimate the muscle mass because of metal implants in the lower extremity among patients with FIF and may impact the accuracy of the test results. Furthermore, this research was not a prospective randomized controlled clinical trial, and the pre-fracture quality-of-life scores of elderly patients with FIF could be determined only after a hospital admission, which inevitably resulted in recall bias. Comparing these scores (EuroQol-5D and IADL) with values from other diseases/studies is also a worthwhile study to be conducted in the future.
Conclusion
Sarcopenia is a risk factor for death and decreased quality of life in elderly patients with FIF within 1 year after surgery, which opens up new avenues for lowering the risk of death and addressing the problem of decreased quality of life in elderly patients with FIF after surgery.