Factors influencing hypothermia in very low/extremely low birth weight infants: a meta-analysis
- Published
- Accepted
- Received
- Academic Editor
- Kazumichi Fujioka
- Subject Areas
- Nursing, Pediatrics
- Keywords
- Very low birth weight infants, Extremely low birth weight infants, Hypothermia, Meta-analysis
- Copyright
- © 2023 Shi et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2023. Factors influencing hypothermia in very low/extremely low birth weight infants: a meta-analysis. PeerJ 11:e14907 https://doi.org/10.7717/peerj.14907
Abstract
Introduction
Previous studies have explored factors that influence the occurrence of hypothermia in very low/extremely low birth weight (VLBW/ELBW) infants, but the factors associated with hypothermia in VLBW or ELBW infants remain inadequately evaluated due to limited prospective data and inconsistency in study populations. Therefore, it is necessary to systematically evaluate the risk factors of hypothermia in VLBW/ELBW infants in order to provide a theoretical basis for clinical practice.
Methods
PubMed and other databases were used to search for case-control or cohort studies on factors influencing the occurrence of hypothermia in VLBW/ELBW infants. The search time was set from database creation to June 30th, 2022. Literature screening, quality evaluation, and data extraction were performed independently by two investigators according to predefined inclusion and exclusion criteria. Meta-analysis was performed using RevMan 5.3.
Results
A total of 10 papers were finally included in this study and 12 factors were established by meta-analysis: body weight (six papers), failure to keep warm in time (three papers), neonatal resuscitation (seven papers), gestational age (three papers), premature rupture of membranes (three papers), maternal combined complications (four papers), cesarean section (six papers), antenatal steroids (four papers), multiple birth (two papers), small for gestational age (two papers), 1 min Apgar score (three papers), and 5 min Apgar score (three papers). Since only one study included race, age (hour), socio-economic status, and spontaneous labor, these factors could not be fitted into RevMan 5.3 for the analysis.
Conclusion
Although there were differences in the study design of the included literature, the influencing factors described in each study were relatively similar. The influencing factors identified in this study may contribute to the construction of related intervention strategies for hypothermia in VLBW/ELBW infants.
Introduction
Neonatal hypothermia is characterized by an abnormal thermal state in which a newborn’s body temperature falls below 36.5 °C (97.7 °F). Its prevalence ranges from 31% to 78% worldwide (Mank et al., 2016; Caldas et al., 2018). Based on core body temperature, the World Health Organization (WHO) categorizes hypothermia into three groups: cold stress (36.0 °C to 36.4 °C, 96.8 °F to 97.5 °F), moderate hypothermia (32.0 °C to 35.9 °C, 89.6 °F to 96.6 °F), and severe hypothermia (<32.0 °C, <89.6 °F) (Feldman et al., 2016). Very low/extremely low birth weight (VLBW/ELBW) infants have a severely limited ability to maintain core body temperature compared to healthy newborns, and so have limited vasoconstriction capacity, higher surface to mass ratio, and less brown fat deposition, which is essential for non-fermentative thermogenesis (Fairchild et al., 2011; Fawcett, 2014). Hypothermia occurs soon following birth in preterm infants, especially in VLBW and ELBW infants, and remains a worldwide problem that can lead to a variety of adverse consequences (Nemeth, Miller & Bräuer, 2021). It has been reported that every 1 °C drop in neonatal body temperature could increase the risk of death by 28% (OR = 1.28, 95% CI [1.16~1.42]) (Laptook et al., 2018) and the occurrence of neonatal hypothermia is significantly associated with the incidence of necrotizing entero-colitis (NEC), intraventricular hemorrhage (IVH), and late-onset sepsis (LOS) (Jakuskiene, Daugeliene & Vollmer, 2009; Shah et al., 2014; Cavallin et al., 2020). Therefore, it is urgent to provide theoretical guidance to improve the survival rate, quality of survival, and administrated direction for VLBW/ELBW infants. Although several works (Almeida et al., 2009; Ali, Osman & Mustafa, 2022; Wilar & Lestari, 2022) have focused on influencing factors, the factors associated with hypothermia of VLBW and ELBW infants remain under-evaluated due to limited prospective data and the inconsistency of the study population. Therefore, there is still a lack of clinical consensus on the risk factors associated with hypothermia due to few existing published studies and recommendations to support healthcare professionals’ decision-making. In this study, we conducted a systematic search for studies on factors influencing the occurrence of hypothermia in VLBW and ELBW infants. Additionally, we performed a meta-analysis of the relevant factors in order to obtain scientifically valid results to guide clinical practice.
Materials and Methods
Literature search and screen
The relevant literature were searched using a combination of subject terms and free words via the databases Embase, Cochrane Library, PubMed, and Web of Science. The search terms were: very low birth weight infant(s), very low birth weight, extremely low birth weight infant(s), hypothermia(s), accidental hypothermia(s), risk, relative risk, cohort studies, cohort. The search time was set from the establishment of the database to June 30, 2022. Inclusion criteria were followed using a clear definition of the concept of hypothermia, VLBW/ELBW infants, and relevant risk factors. Exclusion criteria consisted of normal weight neonates, unavailability of full text, unavailability of Odds Ratio (OR)/Risk Ratio (RR) values for relevant factors, and type of literature (emails, conference articles, reviews, systematic reviews, or meta-analyses). The factors and search terms are shown in Table 1 and detailed search strategies are shown in Appendix 1.
| Factors | Search terms |
|---|---|
| Very low weight infants | ((((“Infant, Very Low Birth Weight”[Mesh]) OR ((((((Very-Low-Birth-Weight Infant[Title/Abstract]) OR (Infant, Very-Low-Birth-Weight[Title/Abstract])) OR (Infants, Very-Low-Birth-Weight[Title/Abstract])) OR (Very Low Birth Weight Infant[Title/Abstract])) OR (Very-Low-Birth-WeightInfants[Title/Abstract])) OR (Very Low Birth Weight[Title/Abstract]))) |
| Extremely low birth weight infant | ((“Infant, ExtremelyLow Birth Weight”[Mesh]) OR (Extremely Low Birth Weight Infant[Title/Abstract]))) |
| Hypothermia | ((“Hypothermia”[Mesh]) OR (((((Hypothermias[Title/Abstract]) OR (Hypothermia, Accidental[Title/Abstract])) OR (Accidental Hypothermia[Title/Abstract])) OR (Accidental Hypothermias[Title/Abstract])) OR (Hypothermias, Accidental[Title/Abstract])))) |
| Risk | ((relative[Title/Abstract] AND risk*[Title/Abstract]) OR (relative risk[Text Word]) OR risks[Text Word] |
| Cohort | cohort studies[MeSH:noexp] OR (cohort[Title/Abstract] AND stud*[Title/Abstract])) |
Date extraction
The literature screening and data extraction were carried out individually by two researchers. Endnote software was used to eliminate duplicate literature, systematic evaluation, review, meta-analysis, and animal experiments. The remaining literature’s titles, abstracts, and full text were read through to complete the secondary screening and ambiguous literature were adjudicated by another researcher. The basic information, study characteristics, and outcome indicators of the literature were extracted by developing a literature extraction form based on the JBI evaluation manual (Peters et al., 2020).
Quality evaluation and risk bias assessment
Since the types of literature included in this study were case-control or cohort studies, the Newcastle-Ottawa Scale (NOS) was used to evaluate the quality (Stang, 2010). This scale assesses the quality level of case-control studies or cohort studies in terms of study population selection, comparability, and exposure (outcome), with a total maximum score of nine. Original literature with a score greater than or equal to six was included in the subsequent meta-analysis. Detailed information on quality assessment and risk bias assessment are provided in Appendix 2.
Analysis
Data analysis was executed using Review Manager 5.3. The RR or OR values were applied as the effect analysis statistic. We calculated a 95% confidence index (CI) for each effect size based on the dichotomous variables of the current study outcome. Moreover, heterogeneity of the enrolled studies was evaluated using a Chi-square test and I2 values. If P > 0.1 and I2 < 50%, it indicated that the heterogeneity among studies was small and it was appropriate to combine effect size using a fixed-effect model; if P < 0.1 and I2 > 50%, it indicated that the heterogeneity among studies was large and it was appropriate to combine effect size using a random-effect model. Begg’s test was used to test the publication bias of the included studies and P < 0.05 was considered statistically significant.
Results
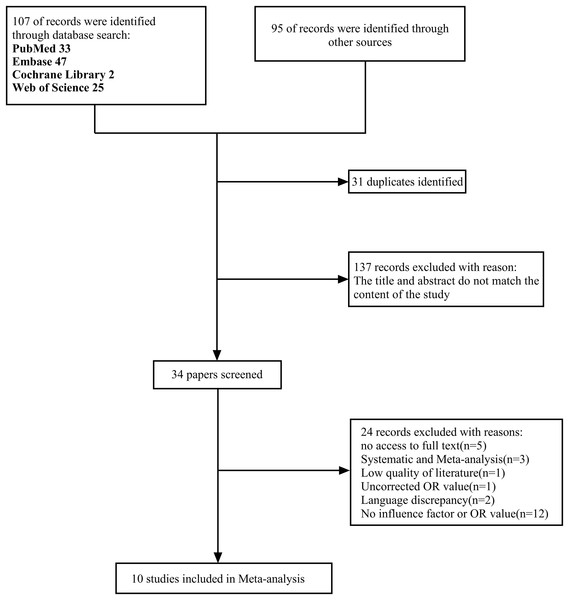
Initially, 202 relevant papers were retrieved, 31 duplicates were excluded by Endnote software, and 137 papers were excluded after reading the titles and abstracts and according to the inclusion and exclusion criteria set for this study. A secondary screening of the remaining 34 papers was performed, and 10 papers were finally included. Reasons for exclusion included unavailability of full text (n = 5), NOS score <6 (n = 1), systematic evaluation and meta-analysis (n = 3), unadjusted OR values (n = 1), language discrepancy (n = 2), and no clearly defined influence factors or OR values (n = 12). The literature screening process is shown in Fig. 1. Because the P value of Begg’s test was greater than 0.05, this demonstrated that the literature included in this study had no publication bias. This study has been registered on the PROSPERO platform under registration number CRD42022342782.
Figure 1: Screening process.
A total of 202 papers were initially obtained, and 10 papers were finally included after double screening.Study characteristics
The basic characteristics of the involved literature are shown in Table 2. Among these 10 studies, five were from China, and the other five studies were from the US, Brazil, Bangladesh, Sweden, and South Korea.
| Inclusion of literature | Country | Type of study | Sample capacity | Influencing factors | NOS score | |
|---|---|---|---|---|---|---|
| Cases | Controls | |||||
| Gao et al. (2022) | China | Case control study | 125 | 122 | ①②③ | 7 |
| Li et al. (2013) | China | Case control study | 181 | 106 | ④⑤⑥⑦ | 7 |
| Zhou et al. (2010) | China | Case control study | 190 | 134 | ①③⑯⑰ | 7 |
| Dong (2021) | China | Case control study | 60 | 40 | ③④⑤⑥ | 7 |
| Yu et al. (2020) | China | Cohort study | 1,100 | 147 | ①③④⑤⑥⑧⑨⑩⑫ | 9 |
| de Almeida et al. (2014) | Brazil | Cohort study | 593 | 754 | ⑦⑨⑩ | 9 |
| Akter, Parvin & Yasmeen (2013) | Bangladesh | Cohort study | 785 | 1,525 | ①③⑤⑬⑭ | 9 |
| Miller, Lee & Gould (2011) | USA | Cohort study | 4,932 | 3,850 | ①②③④⑤⑥⑦⑨⑪⑮ | 9 |
| Wilson et al. (2018) | Sweden | Cohort study | 3,132 | 2,729 | ⑦ | 9 |
| Lee et al. (2019) | Korea | Cohort study | 3,462 | 1,211 | ①③⑤⑥⑧⑨⑩⑫ | 9 |
Note:
① Birth weight; ② Multiple births; ③ Neonatal resuscitation; ④ Antenatal steroids; ⑤ Cesarean section; ⑥ Apgar score; ⑦ Failure to keep warm in time; ⑧ Small for gestational age (SGA); ⑨ Maternal combined complications; ⑩ Gestational age; ⑪ Race; ⑫ Premature rupture of membranes (PROM); ⑬ Newborn age (hour); ⑭ Socioeconomic status; ⑮ Spontaneous delivery; ⑯ Not born in our hospital; ⑰ Born in the cold season.
Meta-analysis results
After data extraction and meta-analysis, a total of 12 factors were summarized in this study: 1 min Apgar score, 5 min Apgar score, small for gestational age (SGA), maternal combined complications, birth weight, multiple births, Cesarean section, premature rupture of membranes (PROM), failure to keep warm in time, neonatal resuscitation, antenatal steroids, and gestational age. As shown in Table 3, we found statistical differences in failure to keep warm in time, neonatal resuscitation, gestational age, maternal combined complications, Cesarean section, and 5 min Apgar score.
| Influencing factors | Study (n) | I2 (%) | Effect model | OR (95% CI) | P |
|---|---|---|---|---|---|
| Body weight | 6 | 92 | Random | 1 [1–1] | 0.32 |
| Failure to keep warm in time | 3 | 86 | Random | 1.97 [1.19–3.28] | 0.008 |
| Neonatal resuscitation | 7 | 75 | Random | 1.86 [1.43–2.43] | <0.001 |
| Gestational age | 3 | 27 | Fixed | 1.1 [1.09–1.1] | <0.001 |
| Premature rupture of membranes | 3 | 0 | Fixed | 1.08 [0.93–1.25] | 0.32 |
| Maternal combined complications | 4 | 85 | Random | 1.28 [1.01–1.62] | 0.04 |
| Cesarean section | 6 | 89 | Random | 1.67 [1.15–2.41] | 0.006 |
| Antenatal steroids | 4 | 88 | Random | 0.78 [0.42–1.44] | 0.42 |
| Multiple birth | 2 | 84 | Random | 1.33 [0.54–3.28] | 0.53 |
| Small for gestational age | 2 | 54 | Random | 1.49 [0.93–2.38] | 0.09 |
| 1 min Apgar score | 3 | 91 | Random | 1.43 [0.96–2.14] | 0.28 |
| 5 min Apgar score | 3 | 65 | 1.47 [1.21–1.78] | <0.001 |
Body weight
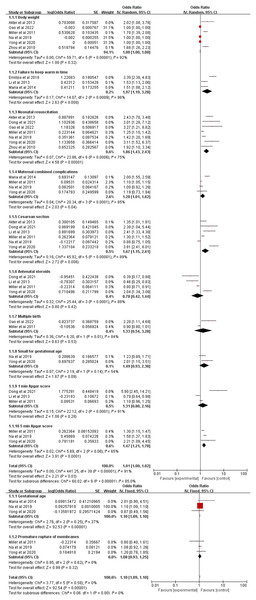
Of the included papers, six involved the effect of body weight on the occurrence of hypothermia (Zhou et al., 2010; Miller, Lee & Gould, 2011; Akter, Parvin & Yasmeen, 2013; Lee et al., 2019; Yu et al., 2020; Gao et al., 2022), and the overall effect (P = 0.32, 95% CI [1.00–1.00]) of body weight on the occurrence of hypothermia was determined to be not statistically different by meta-analysis (Fig. 2).
Figure 2: Forest plot of all influencing factors.
A total of 12 influencing factors were included in the meta-analysis, and the results showed a statistical difference in failure to keep warm in time, neonatal resuscitation, gestational age, maternal combined complications, Cesarean section, and 5 min Apgar score.Failure to keep warm in time
The forest plot for the failure to keep warm in time has also been reported in previous research and three studies (Miller, Lee & Gould, 2011; Li et al., 2013; Wilson et al., 2018) were included in the final analysis (Fig. 2). The forest plot shows that failure to keep warm in time is one of the influencing factors for the occurrence of hypothermia.
Neonatal resuscitation
The results of the meta-analysis of neonatal resuscitation are shown in Fig. 2. In this part, seven studies (Zhou et al., 2010; Miller, Lee & Gould, 2011; Akter, Parvin & Yasmeen, 2013; Lee et al., 2019; Yu et al., 2020; Dong, 2021; Gao et al., 2022) were contained for the final analysis. The OR value for neonatal resuscitation was 1.86 (P < 0.0001, 95% CI [1.43–2.43]).
Gestational age
Three papers (Miller, Lee & Gould, 2011; Lee et al., 2019; Yu et al., 2020) were ultimately selected for the analysis of gestational week on hypothermia (Fig. 2). A fixed effects model was used for the investigation because of high heterogeneity (I2 = 27%). As a consequence, the calculated OR value for gestational age was 1.10 (P < 0.0001, 95% CI [1.09–1.10]).
Premature rupture of membranes
Premature rupture of membranes, a common risk factor for adverse outcomes in both obstetrics and pediatrics, has been shown to be related to the occurrence of hypothermia. Three papers (Miller, Lee & Gould, 2011; Lee et al., 2019; Yu et al., 2020) discussed the effect of premature rupture of membranes on the occurrence of hypothermia (Fig. 2). The results implied no significant difference for premature rupture of membranes on the occurrence of hypothermia (P = 0.32, 95% CI [0.93–1.25]).
Maternal combined complications
Four papers (Miller, Lee & Gould, 2011; de Almeida et al., 2014; Lee et al., 2019; Yu et al., 2020) studied the effect of maternal combined complications on the occurrence of hypothermia. The results indicated that the OR value for maternal combined complications was 1.28 (P = 0.04, 95% CI [1.01–1.62]). The integration results are shown in Fig. 2.
Cesarean section
Six studies (Miller, Lee & Gould, 2011; Akter, Parvin & Yasmeen, 2013; Li et al., 2013; Lee et al., 2019; Yu et al., 2020; Dong, 2021) on Cesarean section were used in our analysis (Fig. 2). The combined results of the random effects model showed that the OR value for Cesarean section was 1.67 (P = 0.006, 95% CI [1.15–2.41]).
Antenatal steroids
The use of antenatal steroids is common, controversial, and has been connected with the occurrence of hypothermia. In this section, four studies (Miller, Lee & Gould, 2011; Li et al., 2013; Yu et al., 2020; Dong, 2021) were recruited for final analysis (Fig. 2). The results showed no significant effect of antenatal steroids on the occurrence of hypothermia after random effects model integration.
Multiple births
Of the 10 included papers, two studies (Miller, Lee & Gould, 2011; Gao et al., 2022) were on the effects of multiple births on hypothermia in VLBW/ELBW infants (Fig. 2). As a result, the OR value for multiple births was 1.33 (P = 0.53, 95% CI [0.54–3.28]).
Small for gestational age (SGA)
Being SGA is associated with many adverse outcomes, including hypothermia. In this article, two studies (Lee et al., 2019; Yu et al., 2020) were included in the meta-analysis (Fig. 2). The forest plot manifested that there was no significant difference for SGA on the occurrence of hypothermia (P = 0.09, 95% CI [0.93–2.38]).
Apgar score
Apgar score is considered a vital indicator for the evaluation of newborns. Five studies (Miller, Lee & Gould, 2011; Li et al., 2013; Lee et al., 2019; Yu et al., 2020; Dong, 2021) were included in the ultimate analysis (Fig. 2). The results showed that a 1 min Apgar score was not statistically significant for the occurrence of hypothermia (P = 0.28, 95% CI [0.8–2.16]), but a 5 min Apgar score was an influencing factor for the occurrence of hypothermia (P < 0.001, 95% CI [1.21–1.78]).
Other factors
Four other relevant factors could not be meta-analyzed because were included in only one study: race 1.3 (1.1~1.5), age 2.25 (1.13~4.47), socio-economic status 2.76 (1.56~4.9), and spontaneous labor 0.8 (0.7~0.9).
Discussion
Failure to keep warm in time involves low room temperature, prolonged time in the room, and no systematic use of hypothermia prevention. Studies have confirmed that for every 2–3 °C drop in deep body temperature, skin temperature drops by 4–6 °C within 30 min of birth. Therefore, to prevent rapid evaporation of heat from newborns, WHO recommends that room temperature should be maintained at 25 °C (Russo et al., 2014). Prolonged time in the room is a risk factor for hypothermia in VLBW/ELBW infants, and may lead to heat evaporation during routine nursing operations and resuscitation due to varying levels of proficiency of health care workers and failure to keep VLBW/ELBW infants warm in a timely manner (Reilly et al., 2015). Hypothermia prevention strategies mainly include the use of polyethylene or polyurethane plastic bags (caps) with variable heat mattresses, and studies have shown that the implementation of these measures can reduce evaporation and transepidermal water loss and maintain constant body temperature by maintaining skin moisture in VLBW/ELBW infants (Sharma et al., 2020).
Neonatal resuscitation includes resuscitation needed, intubation at delivery room, and history of neonatal asphyxia. Neonatal resuscitation may cause hypothermia due to the lack of cerebral blood flow, causing damage of brain tissue and the thermoregulatory center. On the other hand, the main focus of the medical staff during the resuscitation of an infant with asphyxia is on saving the infant’s life, but this may result in prolonged exposure and increased heat evaporation (Zayeri et al., 2007; Ogunlesi et al., 2008).
It has been confirmed that VLBW/ELBW infants have a significant difference in body weight compared to full term infants due to their younger gestational age (Pinheiro et al., 2014). Body weight is closely related to heat production, storage, and thermoregulation in VLBW/ELBW infants. In terms of heat production, these infants have lower birth weight and less brown fat, which is the main source of heat production in infants, and therefore, they do not produce enough heat compared to normal weight infants. The immature development of organs leads to the imperfect development of the thermoregulation center, which aggravates the occurrence of hypothermia (Boo & Guat-Sim Cheah, 2013; Tay et al., 2019).
In the literature we examined, maternal combined complications included gestational hypertension, gestational diabetes mellitus, and chorioamnionitis. Maternal combined complications are often associated with a risk of preterm delivery and related medications, such as hormones and magnesium sulfate, that are used more frequently and can easily lead to muscle relaxation and respiratory depression, increasing the risk of resuscitation and exposure of the child (Greenberg et al., 2011).
The results of this meta-analysis indicated that Cesarean delivery is one of the risk factors for the development of hypothermia in VLBW/ELBW infants, which may be caused by the fact that maternal heat can be generated during the second stage of labor during vaginal delivery by exertion, which promotes the increase of neonatal body temperature. At the same time, the use of anesthetic drugs during Cesarean delivery is not conducive to the recovery of maternal and neonatal thermoregulatory center functions after surgery (Johannsen, Vochem & Neuberger, 2017).
Our meta-analysis suggested that the 5 min Apgar score was a factor influencing the occurrence of hypothermia in VLBW/ELBW infants. Hypothermia may be a result of the neonatal thermoregulatory center being impaired due to asphyxia or other complications. It is also possible that hypothermia is caused by neglecting the application of warming measures during resuscitation (Croop et al., 2020).
Although this study was based on an evidence-based correlation approach to analyze the factors influencing hypothermia in VLBW/ELBW infants, there were several limitations in this meta-analysis. Above all, there was a large heterogeneity across some of the factors. Though we attempted to explore the sources of heterogeneity using subgroup analysis, the effect was minimal. After research and discussion, the reasons may be as follows: first, there were differences in the diagnosis of hypothermia among studies. Although WHO proposed a threshold of 36.5 °C for hypothermia, some of the studies used 36.0 °C or 35 °C as the threshold, which increased the heterogeneity among studies due to different inclusion criteria. In addition, there was inconsistency in the way neonatal temperature was measured. Among the included studies, neonatal temperature measurement methods included rectal, axillary and/or skin, and the inconsistency of temperature measurement methods may have led to differences in temperature reporting between studies, thus increasing the heterogeneity of the results of this meta-analysis. On the whole, there were large differences in temperature variation among different ethnic groups. The American Collaboration for Advancing Pediatric Quality Measures (CAPQuaM) confirmed by analyzing data on newborns in New York State that there were differences in temperature variation among different ethnic groups of newborns, and black infants were more likely to have hypothermia compared with white infants (Lawrence, 2016). In the literature included in this study, the studies covered Asian, European, and American populations, and the differences in body mass of different ethnic groups may have affected the OR values of influencing factors in risk prediction models, thus leading to greater heterogeneity. Second, although the overall risk bias of this study was assessed as low by NOS, the different diagnostic criteria for hypothermia among studies made it possible that there was some information bias in this study. At the same time, because the influencing factor meta-analysis methodology only extracted the OR values for analysis, this study team was unable to explore the potential interactions among the influence factors, indicating that the final results of the influence factor analysis may have some confounding bias. Third, the number of included studies was limited, which may lead to imprecise results of the meta-analysis. The reason for this is the special population of VLBW/ELBW infants, which makes it difficult to obtain more clinical cohort data for research and analysis. Furthermore, due to the particularity of the population, relevant research focused on clinical nursing quality improvement projects, and the discussion and quantification of influencing factors were not involved.
Conclusion
Through literature generalization, we determined a total of 16 factors influencing hypothermia in VLBW/ELBW infants. Of these, four influencing factors (race, age, socio-economic status, and spontaneous labor) were included in only one study, and so the meta-analysis was not performed on them. The remaining 12 factors were included in the meta-analysis, and the results showed that failure to keep warm in time, neonatal resuscitation, gestational age, maternal combined complications, Cesarean section and 5-min Apgar score were contributing factors for hypothermia in VLBW/ELBW infants.
Supplemental Information
Search strategy.
The appendix contains search strategies for 4 databases: PubMed, Embase, Cochrane Library and Web of Science.
Quality assessment and bias analysis.
The appendix contains the results of the quality evaluation and risk bias assessment of the included literature.