Application of combined teaching method of case-based-learning and clinical pathway in practical gynecological teaching
- Published
- Accepted
- Received
- Academic Editor
- Sonia Oliveira
- Subject Areas
- Gynecology and Obstetrics, Science and Medical Education, Healthcare Services
- Keywords
- Case-based learning, Clinical pathway, Practical gynecological teaching
- Copyright
- © 2024 Wang et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2024. Application of combined teaching method of case-based-learning and clinical pathway in practical gynecological teaching. PeerJ 12:e17813 https://doi.org/10.7717/peerj.17813
Abstract
Background
To train highly qualified medical talent in 5-year programs and improve students’ analytical and problem-solving abilities, it is necessary to change the traditional teaching method. This study introduces the combined teaching method of case-based learning (CBL) and clinical pathway and evaluates its role in practical gynecological teaching.
Methods
Medical students in a 5-year program who were enrolled in the fourth year were selected as the research subjects; these students were randomized into two groups that separately received either the traditional teaching method or the combined teaching method of CBL and clinical pathway. Before the internship, a questionnaire was administered to explore students’ views of internship in gynecology, and after the internship, the questionnaire was administered to assess the two teaching methods. Furthermore, theoretical and skill tests were performed both before and after the internship.
Results
A total of 206 medical students in a 5-year program who were in their fourth year were enrolled in the study. Students in the experimental group performed significantly better than those in the control group. They performed significantly better in the postinternship test than in the preinternship test (P < 0.001). The questionnaire showed that more students in the experimental group thought that their learning interests, clinical skills, case analysis ability, clinical communication ability, understanding of theoretical knowledge and clinical thinking ability had improved and significantly differed between the two groups (P < 0.05).
Discussion
Compared to traditional teaching methods, combined teaching method of CBL and clinical pathway can elevate students’ academic performance, improve their learning enthusiasm and help promote clinical teachers’ teaching quality. Additionally, this novel method is effective in facilitating the achievement of teaching objectives and improving the quality of talent training. Therefore, the combined teaching method of CBL and clinical pathway should be popularized and applied in gynecological practice.
Introduction
Gynecology is a clinical discipline that attaches equal importance to both theory and practice, while clinical practice represents the key period during which students should transform theoretical knowledge into practice. Traditional practical gynecological teaching is based mainly on observing teachers’ operation and listening to teachers’ lectures, and in this approach, students lack perceptual cognition of diseases, which often affects their understanding of theoretical knowledge (Li et al., 2022). The current consensus holds that the traditional teacher-centered teaching method is inferior to learner-centered teaching and that the clinical competence and professional growth of medical learners can be most effectively facilitated by learner-centered educational methods (Miles, Al-Shudifat & Yousuf, 2021; Sarwar, Aleem & Nadeem, 2020). Hence, the traditional practical teaching approach no longer meets the needs of practical clinical teaching in hospitals. To train highly qualified medical talent and cultivate students’ ability to analyze and solve problems, changing the traditional teaching method has emerged as an urgent task in the reform of practical gynecology teaching.
Case-based learning (CBL) refers to a teaching method that guides students to analyze cases by referring to real or well-designed representative clinical cases (Cen et al., 2021). This approach can promote active learning and help in the development of critical thinking and analysis in undergraduate medical students (McLean, 2016). Currently, many universities have introduced CBL into the medical education process, and it has been proven to help students better interpret theoretical knowledge (Dubey & Dubey, 2017). Due to the significant differences in teachers’ teaching ability (Harman et al., 2015) and to avoid the inconsistencies stemming from teachers using varied teaching programs, we hope to establish a standardized and programmed disease diagnosis and treatment program around which clinical teaching work can be carried out. This leads us to the idea of a clinical pathway. Clinical pathways are defined as “systematic approaches to guide healthcare professionals in managing a specific problem” (Postma & White, 2016). Furthermore, they are effective and efficient approaches that can standardize treatment progress, support patient care, and facilitate clinical decision-making (Sun et al., 2022; Cabana et al., 1999). However, there are few reports on the application of clinical pathways in gynecological clinical teaching. Aspland, Gartner & Harper (2019), Talib, Lax & Reznik (2018) implemented a clinical asthma pathway in resident education and concluded that the clinical pathway could improve trainees’ comfort and knowledge in managing asthma. To our knowledge, no study has investigated the application of a teaching model combining CBL and clinical pathway in gynecological clinical teaching thus far.
Therefore, we designed this study, which took senior undergraduates majoring in clinical medicine as research subjects and employed the combined teaching method of CBL and clinical pathway in practical clinical teaching. The feasibility and effectiveness of the proposed model in the context of practical gynecological teaching is evaluated through theoretical and skill tests as well as questionnaire surveys administered prior to and after the internship. We hypothesized that the adoption of new teaching methods will result in higher teaching quality and students’ satisfaction compared to traditional teaching methods. The specific implementation procedures are reported below.
Materials and Methods
Participants
A total of 206 5-year medical students who were in their fourth year and who participated in a gynecological internship in Jiaxing Maternity and Child Health Care Hospital were enrolled in the study. This study was approved by the ethics committee of Jiaxing Maternity and Child Health Care Hospital (NO. 2021067). All students provided written informed written consent for the study content.
Study design
The students were randomized into two groups during the 4-week gynecological internship. The two groups separately received either traditional teaching (the control group, 102 students) or combined teaching method of CBL and clinical pathway (the experimental group, 104 students). In the control group, the traditional teaching method was adopted, including 1-week outpatient and 3-week inpatient internships. During the outpatient internship, observation of teachers’ operations was the main focus. During the inpatient internship, the students followed the teachers in managing the patients.
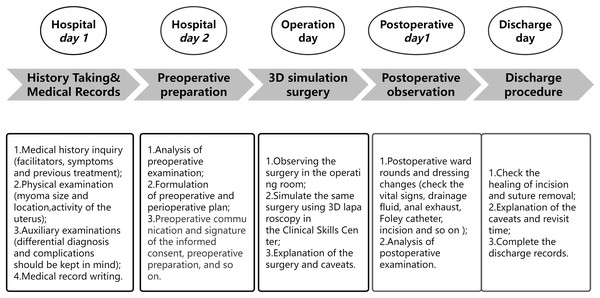
In the experimental group, the combined teaching method of CBL and clinical pathway was employed. The specific process was as follows (examples of uterine leiomyoma teaching, Fig. 1).
Figure 1: Clinical pathway in uterus leiomyoma teaching.
The specific process of combined teaching method of CBL and clinical pathway is shown in the figure. Uterine leiomyoma teaching is shown as an example.
1. Determine the teaching diseases. According to the internship syllabus, common gynecological diseases, such as uterine leiomyoma, adenomyosis, benign ovarian tumor, missed abortion, and ectopic pregnancy were selected as deep learning diseases.
2. Preinternship test and questionnaire survey. The theory test consisted of 50 multiple-choice questions that mainly covered basic knowledge on gynecology, and the skill test was a gynecological examination performed on models. The questionnaire was administered to explore students’ views of internships in gynecology.
3. Independent learning. The teaching secretary sent representative cases and relevant questions related to the teaching disease to students for independent learning in advance. Examples of questions are the following: what are the types of uterine leiomyoma? What are the clinical manifestations of different types? What diseases need to be distinguished from uterine leiomyoma, and how? What are the main diagnostic methods of uterine leiomyoma? What are the treatment methods for uterine leiomyoma? What are the options for medication treatment? What are the indications for surgery? What are the surgical methods? What is the follow-up time and content for various treatment methods?
4. Learn the clinical pathway forms (taking the clinical pathway for surgery of uterine leiomyomas as an example). On the first day of the internship, the clinical teacher explained the clinical pathway form of each teaching disease to the students and emphasized the attention points of each disease.
5. Participate in the teaching clinic. Students followed patients who required hospitalization and met the teaching requirements to the ward.
6. Fully participate in the patient diagnosis and treatment process. According to the Clinical Pathway form and under the guidance of their teacher, students completed patients’ medical history inquiry, physical examination, writing of major medical records, issuing medical orders, preoperative conversation, preoperative preparation, operation observation, and simulating surgery using 3D laparoscope after observation of the surgery, changing the dressing after operation, observing postoperative condition, and discharge records. At this stage, students are required to report patients’ condition to their teacher during daily ward rounds.
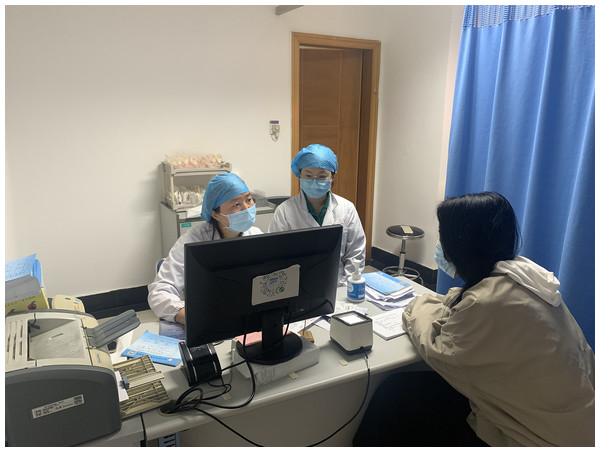
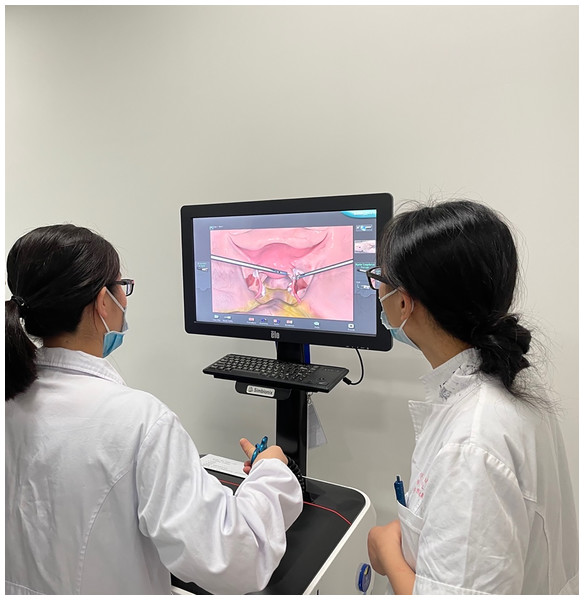
During the 4-week internship period, the students followed the patients from outpatient to inpatient. In the first step in the internship, students followed their teacher to the teaching clinic for observation (Fig. 2) and chose patients who needed hospitalization. Then, the students followed the patient in the whole course of treatment, following the clinical pathway diagnosis and treatment procedures of gynecological disease. The students were required to perform all the clinical work under the teachers’ supervision. “Student-oriented and teacher-guided” ward rounds took place on a daily basis (Fig. 3). The students observed surgical operations and then simulated the surgical operations by using a disease module on a 3D laparoscope (Fig. 4). The time required to treat each patient varied from 3 to 7 days. Finally, the students created and shared courseware for the diseases they diagnosed and treated. All the processes associated with the diagnosis and treatment activities in which they participated were discussed and evaluated holistically. After completing the treatment of one disease, the students proceeded to learn another disease.
7. Case presentation. Weekly discussions were organized for one of the teaching diseases. Students who managed patients with the same disease were required to create a PowerPoint presentation and designate a representative to present it. The students will discuss the disease according to the patients they have managed. The supervising teacher scored and provided feedback based on the presentation and summarized, discussed, and evaluated all the diagnosis and treatment activities in which the students participated. Interns were concurrently guided to conduct literature searches to stay up-to-date with the latest domestic and international research progress in related diseases, enhance their self-study ability, and broaden their horizons.
8. Questionnaire survey. Before the internship, a questionnaire was administered to explore students’ views of internship in gynecology, and after the internship, a questionnaire was administered to assess the two teaching methods. The questionnaires were developed by the researchers following literature review and also drawing from a previous research carried out by the researchers (Talib, Lax & Reznik, 2018; Xu et al., 2023). The first questionnaire contained seven questions, and the second questionnaire contained 12 questions. Information collected using the first questionnaire include: (1) Are you familiar with our internship process? (2) Are you interested in gynecology? (3) Are you confident that you can master gynecological knowledge through internship? (4) Are you willing to participate in the production and explanation of courseware under the guidance of the teacher during the internship? (5) Will you follow the rules and regulations of the internship? (6) Do you think you will become an obstetrician and gynecologist in the future? (7) Do you have any requirements and suggestions for the following internship? Information collected using the second questionnaire include: (1) Your satisfaction with the practice teaching in this department (5 is the most satisfactory). (2) Do you think the learning goals of the internship process are clear? (3) Has your independent learning ability improved during the internship? (4) Has your enthusiasm for learning increased during the internship? (5) Do you think you have improved your oral skills? (6) Do you think it improves the ability of summarization and helps combine textbook knowledge with clinical practice? (7) Do you think it can improve the understanding of the theoretical knowledge? (8) Do you think it can help consolidate clinical knowledge? (9) Do you think it can improve doctor‒patient communication skills? (10) Do you think that the teaching method of CBL combined with clinical pathway takes up too much teaching time, and you prefer to let the teacher explain directly? (11) Do you think it is necessary to carry out more such teaching in the future? (12) Do you have any suggestions for the following internship?
Figure 2: Teaching clinic.
The doctor who is communicating with the patient is a student, and the teacher sitting next to her is observing.Figure 3: Ward rounds.
Students complete daily rounds under the guidance of their teacher. In the picture the student is performing a physical examination on the patient, and the two physicians behind her are her classmates. The teacher standing on the left side of the patient is observing the student’s operation.Figure 4: Simulated surgical operations on a 3D laparoscope.
A student is conducting simulated salpingectomy under the guidance of the teacher.Teaching evaluation
The teaching evaluation consisted of theoretical and skill tests administered both prior to and after the internship as well as questionnaire surveys administered both prior to and after the internship. The theoretical tests each comprised a preinternship test featuring 50 multiple-choice questions and a postinternship test featuring 40 multiple-choice questions, with a total score of 100. The preinternship questionnaire survey focused on students’ views of internships in gynecology, while the postinternship questionnaire survey aimed to explore students’ perceptions and views during the practical teaching process. In the skills test, the examiners were blinded to the cohort they were examining. The test and questionnaire survey results for the two groups of students were compared to evaluate the improvement effect of the novel teaching model, thereby providing data support for the further improvement of subsequent teaching approaches.
Statistical methods
Data were statistically processed using SPSS 21.0 software 2 (IBM, Armonk, NY, USA). The data thus measured that followed a normal distribution were expressed as x ± s, and their intergroup comparison was performed using a t test. The enumeration data were expressed in terms of rates and compared using the X2 test. Differences were considered statistically significant when P < 0.05.
Results
General situation of students in the two groups (Table 1)
A total of 206 students participated in the present teaching research across the two groups. The experimental group comprised 104 students receiving combined teaching method of CBL and clinical pathway, including 48 females and 56 males with a mean age of 22.48 ± 0.56 years. The control group comprised 102 students receiving traditional teaching method, including 49 females and 53 males with a mean age of 22.45 ± 0.52 years.
| Variable | The control group (n = 102) | The experimental group (n = 104) | P | |
|---|---|---|---|---|
| Age/year | 22.45 ± 0.52 | 22.48 ± 0.56 | 0.769 | |
| Gender | Female | 49 (48.04%) | 48 (46.15%) | 0.786 |
| Male | 53 (51.96%) | 56 (53.85%) | ||
| Theoretical test scores | 70.65 ± 9.49 | 70.77 ± 9.54 | 0.927 | |
| Skill test scores | 79.91 ± 5.92 | 79.58 ± 4.24 | 0.642 | |
| Familiar with the internship process | Yes | 89 (87.25%) | 87 (83.65%) | 0.464 |
| No | 13 (12.75%) | 17 (16.35%) | ||
| Being interested in gynecology | Yes | 56 (54.90%) | 55 (52.88%) | 0.772 |
| No | 46 (45.10%) | 49 (47.12%) | ||
| Being confident in one’s mastery of gynecological knowledge | Yes | 92 (90.20%) | 90 (86.54%) | 0.413 |
| No | 10 (9.80%) | 14 (13.46%) | ||
Note:
A mixture of demographic data, student performance data and data from the pre-internship questionnaire. Data are expressed as mean ± SD/(range)or as frequency [i] (%).
There was no significant difference between the two groups. Questionnaire surveys were administered prior to the internship, and most of the students in the two groups were familiar with the internship process and were confident in their mastery of gynecological knowledge. Only half of the students in the two groups were interested in gynecology. There was also no significant difference between the groups. The mean theoretical test score of the experimental group was 70.77 ± 9.54, and that of the control group was 70.65 ± 9.49. The skill test score of the experimental group was 79.58 ± 4.24, and that of the control group was 79.91 ± 5.92. No significant difference was found in terms of participants’ preinternship test scores (P > 0.05).
Comparison of students’ scores between the two groups (Table 2)
In the experimental group, the mean skill test score and the mean theoretical test score were 94.33 ± 3.53 and 88.39 ± 6.45 in the postinternship test and 79.58 ± 4.24 and 70.77 ± 9.54 in the preinternship test, respectively. In the control group, the scores were 88.91 ± 5.39 and 81.38 ± 7.60 in the postinternship test and 79.91 ± 5.92 and 70.64 ± 9.49 in the preinternship test. Students in the experimental group performed significantly better than those in the control group. They performed significantly better in the postinternship test than in the preinternship test (P < 0.001). At the same time, the questionnaire showed that more students in the experimental group thought their learning interests, clinical skills, case analysis ability, clinical communication ability, understanding of theoretical knowledge and clinical thinking ability had improved, and the difference was statistically significant (P < 0.05).
| Theoretical test scores | Skill test scores | Total scores | The improvement of theoretical test scores | The improvement of skill test scores | ||||
|---|---|---|---|---|---|---|---|---|
| Before internship | After internship | Before internship | After internship | Before internship | After internship | |||
| The control group (n = 102) | 70.64 ± 9.49 | 81.38 ± 7.60 | 79.91 ± 5.92 | 88.91 ± 5.39 | 150.56 ± 13.83 | 170.29 ± 11.21 | 10.74 ± 5.42 | 9.00 ± 4.05 |
| The experimental group (n = 104) | 70.77 ± 9.54 | 88.39 ± 6.45 | 79.58 ± 4.24 | 94.33 ± 3.53 | 150.35 ± 12.02 | 182.72 ± 9.52 | 17.63 ± 5.60 | 14.75 ± 4.50 |
| P | 0.927 | <0.001 | 0.642 | <0.001 | 0.906 | <0.001 | <0.001 | <0.001 |
Note:
A comparison of students’ theoretical and skill test scores variables before and after internship, as well as a comparison of the improvement of theoretical and skill test scores.
The increase in theoretical test scores from postinternship to preinternship in the experimental group was 17.63 ± 5.60, and in the control group, it was 10.74 ± 5.42. The increase in skill test scores from postinternship to internship in the experimental group was 14.75 ± 4.50, and in the control group, it was 9.00 ± 4.05. The improvement in test scores in the experimental group was significantly greater than that in the control group, and the difference was statistically significant (P < 0.05).
Comparison of postinternship questionnaire survey results between the two groups (Table 3)
In this research, 206 valid questionnaires were collected from the students. The experimental group had clearer learning goals. In total, 88.46% of students in the experimental group believed that improved independent learning ability after the internship; this proportion was 65.68% in the control group, and the difference was statistically significant (P < 0.001). A total of 82.69% of students in the experimental group believed that their doctor–patient communication skills had improved, while this proportion was only 56.86% in the control group. Students in both groups believed that their internships could effectively enable them to connect book theories with clinical practice. However, students in the experimental group believed that their internships were more conducive to the understanding and consolidation of knowledge. Satisfaction with practical teaching was higher in the experimental group than in the control group, and the difference was statistically significant (P < 0.001).
| Attitude to the process of internship | The control group (n = 102) |
The experimental group (n = 104) | P |
|---|---|---|---|
| Clear learning goals | 71 (69.61%) | 89 (85.58%) | 0.006 |
| Improve independent learning ability | 67 (65.68%) | 92 (88.46%) | <0.001 |
| Improve learning enthusiasm | 78 (76.47%) | 93 (89.42%) | 0.013 |
| Help combine textbook knowledge with clinical practice | 84 (82.35%) | 90 (86.54%) | 0.407 |
| Improved understanding of theoretical knowledge | 58 (56.86%) | 86 (82.69%) | <0.001 |
| Help consolidate clinical knowledge | 54 (52.94%) | 78 (75.00%) | 0.001 |
| Improve doctor–patient communication skills | 58 (56.86%) | 86 (82.69%) | <0.001 |
| Satisfaction with internship* | 3.69 ± 0.82 | 4.80 ± 0.61 | <0.001 |
Notes:
A questionnaire analysis of the students’ attitudes towards the internship process after the internship.
Discussion
The combined teaching method of CBL and clinical pathway improves teaching quality
Teachers are always busy with clinical work and pay little attention to teaching effect and quality (Peng et al., 2018; Chaou et al., 2019). By establishing the clinical pathway of diseases, we established a standardized and programmed disease diagnosis and treatment plan and organized clinical teaching work around this plan to avoid the inconsistencies in different teachers’ teaching programs. We specified the content and operational highlights that interns need to master from the first day of admission to discharge for patients with each disease. These regulations not only standardize the teaching process but also enhance the systematicness of the teaching content, which is beneficial for interns to more objectively understand and master the scientific diagnosis and treatment of diseases and for students to form a systematic clinical knowledge structure. During the diagnosis and treatment of real patients, students can closely grasp the primary aspects of diagnosis, differential diagnosis, and treatment, develop correct clinical thinking modes, and strengthen their perceptual and rational understanding of clinical diagnosis and treatment activities. The results of this study showed that the theoretical test and skill operation scores of the experimental group after the internship were higher than those of the control group. A previous study also concluded that after the implementation of clinical pathways, residents’ knowledge and preparedness to manage asthma improved (Talib, Lax & Reznik, 2018).
The combined teaching method of CBL and clinical pathway improves the learning initiative of students
The combined teaching method of CBL and clinical pathway advocates the teaching approach that places students as the primary actors and teachers in the role of facilitators. Before the internship, the teaching secretary sent representative cases and relevant questions related to the teaching disease to students for independent learning in advance. These cases combine theory with practice, enabling students to apply knowledge to cases and prepare them for clinical practice. During the internship, teachers regularly provide guidance to students to diagnose and treat actual patients in all aspects of the clinical pathway, which greatly enhances students’ initiative in self-directed learning and stimulates their ability for critical clinical thinking to identify and solve problems. With the theoretical foundation and guidance in students’ clinical path, students gain the skills to proactively engage in communication with patients, which improves their doctor‒patient communication ability and enhances their self-confidence. Weekly case discussions ensure that students approach each patient with due diligence. It is only through careful analysis that students can summarize the diagnosis and treatment process, as well as the overall clinical decision-making process, into a PowerPoint presentation. In the event of any unique situations arising during the diagnosis and treatment process, students are also expected to consult literature resources, thereby deepening their level of engagement and enhancing their learning initiative. In our study, 88.46% of the experimental group students believed that the new teaching method improved their ability to learn independently. A total of 89.42% of the students in the experimental group thought that the new teaching method improved their learning enthusiasm, which was significantly higher than that of the control group (76.47%).
The combined teaching method of CBL and clinical pathway have significantly improved students’ diagnosis skills
The clinical pathway refers to the establishment of a standardized treatment model and protocol for a specific disease, which is a comprehensive model related to clinical practice. Guided by evidence-based medical evidence and clinical guidelines, it promotes treatment organization and disease management methods, ultimately playing a role in standardizing medical practices, reducing variation and costs, and improving quality (Buchert & Butler, 2016). Combining clinical pathways with teaching allows for the integration of teaching into clinical work, making it easier for students to master the diagnosis and treatment of diseases in clinical practice, with stronger relevance, clearer teaching content, and greater flexibility in teaching methods. The history-taking process greatly develops students’ doctor–patient communication skills, the formulation of treatment plans trains students’ clinical thinking ability, and postoperative observation deepens students’ overall understanding of the disease. Therefore, applying clinical pathways to teaching can enable interns to quickly enter the working state and effectively complete their internship tasks. This effective learning method enables them to more quickly and efficiently grasp the key points of diagnosis and treatment of various diseases, thus enabling the experimental group students to achieve higher scores on various exams and obtain better learning results, thereby improving teaching quality. In 1995, the American Journal of Internal Medicine reported that Harvard Medical School and other institutions applied clinical pathway management methods to teaching, This innovative method, when combined with other teaching methods, greatly improved the clinical hands-on ability of interns and achieved good results (Pearson, Goulart-Fisher & Lee, 1995). A total of 82.69% of the students in the experimental group thought that the new method improved their understanding of theoretical knowledge, which was significantly higher than that of the control group.
The combined teaching method of CBL and clinical pathway can enhance the satisfaction of students
Traditional teaching methods often result in teachers being busy with clinical work and neglecting students. After completing teaching rounds, students have nothing to do, and some read books or play on their mobile phones in the demonstration classroom (Xu et al., 2023). Teachers only take care of weekly teaching activities, leaving students in a passive state. The combined teaching method of CBL and clinical pathway standardizes the teaching process, and teachers shift from “teaching medical knowledge” to “teaching learning methods”. The new teaching process is student-centered, teacher-guided and uses a powerful tool-clinical pathway. Using the new teaching method, students fully participated in the whole treatment process, and they could freely express their views. The new teaching method can also exercise students’ abilities in various aspects, such as literature retrieval, summarization, comprehensive understanding, and oral expression skills, and can cultivate their clinical thinking ability, improve their comprehensive analysis ability, and enhance their spirit of teamwork. Additionally, due to the deepening of the concept of minimally invasive interventions, laparoscopy has been widely used and has come to represent an important aspect of fast-track surgery development (Wang, 2021). In the new teaching method, we also give students chances to simulate surgery using a 3D laparoscope after observation of the surgery. These factors have transformed the situation of students being idle in traditional teaching methods and improved their satisfaction. In our study, the score of students’ satisfaction with the internship in gynecology was 4.8 ± 0.61, which was significantly higher than the score of students in the control group.
Shortcomings
Currently, the clinical course of many diseases is complex, with numerous variations and uncertainties, and some diseases cannot be treated with clinical pathway therapy. Therefore, it is necessary for teachers to integrate the new teaching method with existing medical resources and conditions and choose appropriate teaching patients to achieve the best teaching effect.
Conclusions
In summary, the combined teaching method of CBL and clinical pathway plays a positive leading role in enabling clinical medical students to embrace new single-disease quality control concepts, cultivate standardized, normalized, and scientific clinical thinking methods, and acquire comprehensive and systematic modern medical knowledge. The authors believes that integrating typical cases and clinical pathways into clinical practice teaching can improve the overall quality of clinical teaching.
Supplemental Information
English version of the questionnaires.
Before the internship, a questionnaire was administered to explore students’ views of internship in gynecology, and after the internship, the questionnaire was administered to assess the two teaching methods.
Chinese version of the questionnaires.
Before the internship, a questionnaire was administered to explore students’ views of internship in gynecology, and after the internship, the questionnaire was administered to assess the two teaching methods.