Evaluating exercise therapies in adolescent idiopathic scoliosis: a systematic review with Bayesian network meta-analysis
- Published
- Accepted
- Received
- Academic Editor
- Jincheng Wang
- Subject Areas
- Kinesiology, Orthopedics, Biomechanics, Rehabilitation, Sports Medicine
- Keywords
- Adolescent Idiopathic Scoliosis, Scoliosis, AIS, Exercise therapies, Exercise, Network meta-analysis
- Copyright
- © 2025 Jiang et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits using, remixing, and building upon the work non-commercially, as long as it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2025. Evaluating exercise therapies in adolescent idiopathic scoliosis: a systematic review with Bayesian network meta-analysis. PeerJ 13:e19175 https://doi.org/10.7717/peerj.19175
Abstract
Background
Exercise therapy represents a financially prudent and readily applicable intervention that has gained considerable traction in the treatment of adolescent idiopathic scoliosis (AIS) in recent years. Nevertheless, a definitive agreement on the superiority of one method over another remains elusive.
Methods
A comprehensive search was performed across the PubMed, Cochrane Library, Embase, and Web of Science databases for randomized controlled trials pertaining to exercise and AIS, concluding on August 20, 2024. Four independent researchers conducted a thorough review of the literature, engaged in meticulous data extraction, and assessed the risk of bias. A Bayesian network meta-analysis was performed utilizing the R programming language (version 4.3.4) and MetaInsight tool (version V6.0.1).
Results
A total of 23 studies were incorporated into the analysis, encompassing 1,289 participants with AIS. Compared to the control group, the primary meta-analysis showed that both SchrothCo and physiotherapeutic scoliosis-specific exercises (PSSE) modalities significantly improved Cobb angle (MD = −4.79, 95% CI [−8.56 to −1.11] MD = −3.11, 95% CI [−5.27 to −0.9]), axial trunk rotation (ATR) (MD = −3.03, 95% CI [−4.68 to −1.46]; MD = −2.37, 95% CI [−3.59 to −1.14]), and SRS-22 scores (MD = 0.66, 95% CI [0.39–0.94]; MD = 0.44, 95% CI [0.22–0.66]). The secondary meta-analysis showed that within the PSSE modality, Schroth therapy significantly reduced Cobb angle (MD = −2.3, 95% CI [−5.45 to −0.66]), while in the SchrothCo modality, both Schroth + Core and Schroth + Hippotherapy significantly improved Cobb angle (MD = −5.27, 95% CI [−14.15 to −3.5]). For ATR, Schroth therapy within PSSE (MD = −2.79, 95% CI [−6.4 to −0.1]), and Schroth + Core (MD = −4.03, 95% CI [−9.37 to −0.98]), Schroth + Sling (MD = −3.12, 95% CI [−10.05 to −2.94]), and Schroth + Hippotherapy (MD = −3.39, 95% CI [−10.29 to −2.84]) within the SchrothCo modality all showed significant reductions. Significant differences in SRS-22 scores were found only in the PSSE modality with Schroth therapy (MD = 0.48, 95% CI [0.02–0.9]) and in the SchrothCo modality with Schroth + Core (MD = 0.79, 95% CI [0.13–1.43]).
Conclusions
According to the latest findings, the integration of the Schroth method with core stabilization training (Schroth + Core) is regarded as the optimal strategy for addressing AIS. The integration of core stabilization training with the Schroth method reveals a markedly enhanced effectiveness. Future inquiries should encompass more rigorous studies to establish a more robust evidence foundation and facilitate progress in this domain.
Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional spinal deformity that occurs during growth and development, characterized by asymmetric curvature and rotational deformity of the spine, with idiopathic cases accounting for up to 90% of all cases (Abdel-aziem et al., 2021). A Cobb angle ≥ 10° on a standing full-spine X-ray is diagnostic for scoliosis (Kuznia, Hernandez & Lee, 2020). Epidemiological studies indicate that AIS predominantly affects individuals between the ages of 10 and 16, with an incidence rate of 2%–12% and a higher prevalence in females (Chen et al., 2016; Urrutia, Besa & Bengoa, 2018; Negrini et al., 2018; Ekşi et al., 2020; Xu et al., 2024). However, the exact pathogenesis of AIS remains poorly understood. Research suggests that AIS arises from a complex interplay of multiple factors, including genetic predisposition, spinal biomechanics, neurology, hormonal regulation, biochemistry, environmental influences, and the combined effect of both internal and external behavioral changes (Peng et al., 2020; Marya et al., 2022). Furthermore, scoliosis in adolescents can lead to complications such as back pain, respiratory issues, disability, and mental health problems, all of which can significantly impair their quality of life (Danielsson et al., 2003; Romano et al., 2013; Jinnah et al., 2024). These complexities pose substantial challenges for the clinical diagnosis, management, and rehabilitation of AIS.
Treatment can be categorized into surgical and non-surgical approaches, informed by the distinct stages of AIS progression. The International Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) guidelines (Negrini et al., 2018) advocate for AIS patients exhibiting a Cobb angle ranging from 10 to 45 degrees to pursue a regimen of bracing in conjunction with exercise therapy, rather than opting for surgical intervention. In contrast to extended brace usage, which can lead to discomfort, noncompliance, and a diminished quality of life (Negrini et al., 2015; Hawary et al., 2019), exercise therapy presents a multitude of advantages for patients with AIS. These benefits encompass affordability, negligible side effects, improved aesthetic perception, and an overall enhancement in quality of life (Weinstein et al., 2008; Gámiz-Bermúdez et al., 2022; Yildirim et al., 2022). Currently, the most commonly used exercise therapy in clinical practice is Physiotherapeutic Scoliosis-Specific Exercises (PSSE), which includes various specific exercise methods such as Schroth, Scientific Exercise Approach to Scoliosis (SEAS), Barcelona Scoliosis Physical Therapy School (BSPTS), Functional Individual Treatment for Scoliosis (FITS), Lyon, Side Shift, and DoboMed (Seleviciene et al., 2022). Additionally, core stabilization training, suspension training, and balance training, as well as Pilates and proprioceptive neuromuscular facilitation (PNF) training, are also widely implemented in clinical practice (Ma et al., 2023b; Baik, Kim & Lee, 2023; Romano et al., 2024). Notably, in recent years, there has been a growing trend of combining PSSE with other forms of exercise therapy (Dong et al., 2025), offering a more comprehensive and varied rehabilitation approach. This integrated therapeutic strategy has shown greater efficacy in alleviating symptoms and improving overall quality of life.
While exercise therapies have shown beneficial clinical outcomes, reaching a consensus on the most effective intervention continues to be a challenge, and current guidelines do not provide definitive instructions. Several meta-analyses have compared the effects of exercise therapies on AIS (Dimitrijević et al., 2022; Ceballos-Laita et al., 2023; Chen et al., 2024), focusing on changes in the Cobb angle and highlighting the importance of assessing patient-related outcomes emphasized by SOSORT, such as the angle of trunk rotation (ATR) and quality of life. Prior research has concentrated on evaluating the effectiveness of the PSSE system compared to conventional treatment approaches. It appears that studies exploring distinctions in therapeutic outcomes across different exercise therapies are still relatively limited. This study aims to fill the existing research gap by systematically reviewing published randomized controlled trials (RCTs) concerning exercise interventions for AIS. Furthermore, it utilizes Bayesian network meta-analysis to assess and compare the rehabilitation effects of various exercise therapies. The objective is to furnish the most robust evidence-based recommendations for the management of AIS.
Materials and Methods
This investigation adheres meticulously to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Page et al., 2021), thereby guaranteeing the transparency and rigor of the research methodology employed. We have preregistered on the PROSPERO platform to bolster the credibility and reproducibility of the study, with the registration number: CRD42024571578.
Literature retrieval strategy
A thorough and methodical database search strategy was developed to pinpoint randomized controlled trials (RCTs) that detail the effectiveness of various exercise therapies for individuals suffering from adolescent idiopathic scoliosis. The comprehensive investigation included the PubMed, Embase, Cochrane Library, and Web of Science databases. Three investigators (YJ, HP, and YY Song) independently conducted literature searches following the established search criteria. Any disagreements concerning study inclusion were resolved through consultation with a fourth investigator (NY). The search strategy was devised in accordance with Boolean logic, employing a blend of free-text terms and Medical Subject Headings (MeSH) to guarantee thoroughness and precision. The duration for searching has been prolonged from the establishment of each database until August 20, 2024, without the implementation of any search filters or limitations. The terms employed in the investigation comprised: “Scoliosis” OR “Idiopathic scoliosis” OR “Adolescent idiopathic scoliosis” AND “Adolescent” AND “Exercise” OR “Movement” OR “Training” OR “Motion” OR “Physiotherapeutic scoliosis specific exercises” (Supplemental Information).
Inclusion criteria
The criteria for inclusion and exclusion were established in accordance with the PICOS framework. Inclusion criteria: (1) Participants: Male or female adolescents, aged 10 to 18 years, with a Cobb angle ranging from 10° to 45°, who have not undergone surgical treatment and have no restrictions related to scoliosis classification, disease progression, or other medical conditions. Participants must not have engaged in large-scale physical activities during the six months prior to the experiment. (2) Interventions: Research examining the effects of exercise interventions on AIS. The control group will receive no intervention, standard of care, brace correction, or a waiting list control. To assess the effectiveness of a specific exercise therapy, the experimental group will undergo exercise therapy in addition to the control group interventions. The exercise therapies include PSSE, strengthening training, Pilates, and PNF training, with the possibility of combining these therapies. (3) Comparative analyses: Evaluations of distinctions among various exercise intervention cohorts or between exercise intervention cohorts and non-exercise control cohorts. (4) Outcomes: Documenting variations in Cobb angle, axial trunk rotation (ATR), or the Scoliosis Research Society-22 (SRS-22) questionnaire prior to and following the intervention. Studies included in this analysis must present at least one of the specified outcomes. (5) Types of studies: Exclusively randomized controlled trials. (6) Publication channels: This analysis exclusively includes studies that have undergone the rigorous process of peer review and are published in English-language journals.
Exclusion criteria
(1) Non-randomized controlled trials. (2) The detailed protocols of the intervention methods for the control and experimental groups were not reported in detail. (3) Investigations that incorporate additional simultaneous interventions alongside exercise, including nutritional supplements or alterations in medication. (4) Animal studies, abstracts, reviews, conference reports, and similar scholarly materials. (5) Full text that is not accessible, absent data, or data that cannot be retrieved.
Study selection
The EndNote X9.1 software was employed to eliminate duplicate and irrelevant studies that failed to satisfy the inclusion criteria. To uphold the rigor of the research, YPS and LH performed a meticulous manual cross-examination of distinct studies. Following this, two scholars (YJ and PCL) conducted a thorough examination of the literature by initially assessing titles and abstracts, which was succeeded by a comprehensive review of the full texts, during which they independently extracted data from the chosen studies. All discrepancies were addressed through mutual agreement; if required, a third reviewer (HBC) was engaged for mediation. Comprehensive documentation of the criteria for inclusion or exclusion was meticulously preserved. This study explicitly excluded case reports, letters, and conference abstracts. The entire process was documented and summarized in a PRISMA flow diagram to ensure transparency and traceability.
Data extraction
Two researchers (YJ and GSY) will carefully examine the complete texts of the studies included and systematically extract the required information according to a standardized protocol. The data to be extracted will encompass the name of the first author, the year of publication, the design of the study, the age and gender of participants, the size of the sample, and the characteristics of the intervention, which include its content, methods, and duration. Furthermore, we will extract outcome measures after exercise interventions, including the Cobb angle, ATR, and SRS-22 scores. In the event that disagreements emerge during the data extraction process, a third researcher (QGC) will be solicited to participate in the discourse until a consensus is achieved, thereby safeguarding the accuracy of the data and the integrity of the study’s findings.
(1) Calculate the mean difference (MD) of changes before and after the intervention using the following formula (Cumpston et al., 2019): (2) Calculate the standard deviation (SD) of changes before and after the intervention using the following formula (Cumpston et al., 2019):
Risk of bias and quality of evidence
In accordance with the Cochrane risk of bias assessment guidelines (Cumpston et al., 2019), the evaluation of bias risk in the included studies was conducted by two researchers (YJ and LH). The researchers conducted a thorough analysis of each assessment domain, addressing any discrepancies through the consultation of a third researcher (NY). We assessed the potential for bias in the included studies utilizing the second iteration of the Risk of Bias tool (RoB 2) (Sterne et al., 2019). The evaluation encompassed several critical dimensions: the process of randomization, deviations from the intended interventions, the handling of missing outcome data, the measurement of outcomes, the selection of reported results, and an overarching assessment of bias.
Statistical analysis
This research employed R software (version R 4.3.3) alongside the BUGSnet and gemtc packages for the purposes of statistical analysis and graphical representation. Additionally, the MetaInsight tool (version V6.0.1) was used to assist in generating charts (Owen et al., 2019). Bayesian methodologies were utilized for the selection of effect models, and the evaluation of model fit was conducted through the deviance information criterion (DIC), where reduced DIC values signify an improved model fit (Béliveau et al., 2019). Considering the observed heterogeneity, the choice was made to employ either a fixed-effect model or a random-effect model; should the heterogeneity prove to be significant, the random-effect model would be utilized, whereas a fixed-effect model would be applied in its absence (Halme, McAlpine & Martini, 2023). For effect size selection, all indices were continuous variables, represented as mean difference (MD) and their 95% credibility interval (CI). The ranking of exercise therapy interventions was assessed using the Surface Under the Cumulative Ranking Curve (SUCRA), with higher SUCRA values indicating better efficacy (Nevill, Cooper & Sutton, 2023). Bayesian network meta-analysis was performed using the nma.run() function, network relationship diagrams were drawn using the net.plot() function, and treatment ranking results were generated with the nma.rank() function. Additionally, SUCRA and rankogram charts were used to predict the ranking probabilities of various interventions, and ranking league diagrams were generated using the nma.league() function. Based on the characteristics of subjects included in the literature and the results of NMA, we conducted regression analyses using the gemtc packages on covariate factors that might influence the combined primary effects. The regression coefficients (β) and 95% confidence intervals were utilized to assess the significance of their moderating effects (Shim et al., 2019). The assessment of heterogeneity was conducted utilizing the I2 statistic, where I2 values under 25% in Cochran’s Q test are regarded as indicative of low heterogeneity (Huedo-Medina et al., 2006). Should this threshold be surpassed, subsequent analyses including Egger’s regression test (1997) were conducted to assess the symmetry of the funnel plot and the possibility of publication bias (Egger et al., 1997).
A standalone network meta-analysis (NMA) was conducted, categorized by primary exercise therapy modalities (PSSE modality, SchrothCo modality, Pilates exercise, intensive training, and PNF training). This was further analyzed using secondary exercise subgroups (Schroth, BSPTS, SEAS, and Lyon were grouped under PSSE modalities; Schroth combined with sling training, balance training, hippotherapy, and core stability training were grouped under Schroth Combo modalities; while core stability training and sling training were grouped under the strengthening training group). A network diagram was created to visually present both the direct and indirect comparisons between different therapeutic modalities. The NMA results were reported as mean effects with 95% credible intervals. A rank probability analysis was conducted to generate surface under the cumulative ranking curve (SUCRA) values for each primary exercise modality and subgroup, which were visually presented using Litmus Rank-O-Gram SUCRA plots or Radial SUCRA plots.
Evidence grade evaluation
The CINeMA tool was employed for the assessment of evidence grading. This instrument, developed by the Cochrane group, is grounded in a GRADE adaptation tailored for network meta-analysis, particularly aimed at the comparison of various interventions (Nikolakopoulou et al., 2020). In accordance with the established guidelines, two researchers (YJ and NY) evaluated within-study bias, between-study bias, indirectness, imprecision, heterogeneity, and inconsistency for each comparison.
Results
Literature screening results and study characteristics
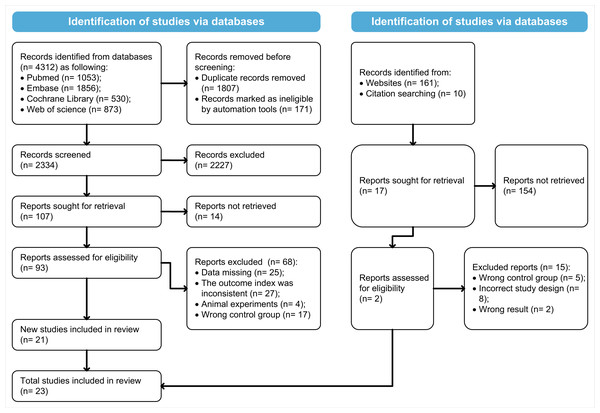
Following a methodical exploration of four databases, 4,312 articles were obtained. Upon the elimination of duplicates, 2,334 records remained. Following a meticulous examination of titles and abstracts, 2,227 articles that did not pertain to the study were excluded. A comprehensive full-text review resulted in the exclusion of an additional 68 articles for several reasons: absence of data (n = 25), incongruent outcome measures (n = 27), studies involving animals (n = 4), and inappropriate control groups (n = 17), yielding 21 studies for consideration. Furthermore, two additional articles were discerned through a meticulous search on Google Scholar and the process of reference tracking. A total of 23 studies (Monticone et al., 2014; Kim & HwangBo, 2016; Kuru et al., 2016; Ko & Kang, 2017; Yu, Yang & Park, 2019; Negrini et al., 2019; Yagci & Yakut, 2019; Zapata, Sucato & Jo, 2019; Schreiber et al., 2019; Kocaman et al., 2021; Won, Oh & Shen, 2021; Gao et al., 2021; Mohamed & Yousef, 2021; Abdel-aziem et al., 2021; El et al., 2022; Qi et al., 2022; Zapata et al., 2023; Shen et al., 2023; Khaledi et al., 2024; Manzak Dursun et al., 2024; Zhang et al., 2024; Karavidas et al., 2024; Büyükturan et al., 2024) were incorporated into the network meta-analysis. See Fig. 1 for details.
Figure 1: The preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow chart.
A total of 1,289 subjects with AIS were encompassed within the 23 studies included in the analysis. The control group will not receive any interventions, standard care, brace correction, or be placed on a waiting list. Considering the attributes of the studies examined, the interventions within the experimental groups were categorized into distinct primary treatment modality groups, including PSSE modality, SchrothCo modality, Pilates exercises, sling training, and PNF training. Schroth, BSPTS, SEAS, and Lyon were identified as PSSE modalities. The combinations of Schroth with sling training, balance training, hippotherapy, and core stability training were designated as SchrothCo modalities. Meanwhile, core stability training and suspension training were classified as intensive training groups (Table 1).
| Study design | Country | Participant | Treatment | Samplesize | Gender (male/female) /n | Age | Duration (weeks) | Outcome index | |
|---|---|---|---|---|---|---|---|---|---|
| Zhang et al. (2024) | RCT | China | adolescents | T1: Schroth | 29 | 5/24 | 13.97 ± 1.21 | 12 | ①②③ |
| T2: Schroth + Sling | 31 | 7/24 | 13.42 ± 1.06 | 12 | |||||
| Manzak Dursun et al. (2024) | RCT | Turkey | adolescents | C: Standard of care | 15 | 0/15 | 10-18 | 12 | ①② |
| T: Pilates | 16 | 1/15 | 10-18 | 12 | |||||
| Khaledi et al. (2024) | RCT | Iran | adolescents | C: Waiting list control | 10 | 10/0 | 15.4 ± 1.51 | 12 | ①②③ |
| T1: Schroth | 15 | 15/0 | 16.27 ± 1.44 | 12 | |||||
| T2: Schroth + Core | 15 | 15/0 | 16.33 ± 0.90 | 12 | |||||
| Karavidas et al. (2024) | RCT | Greece | adolescents | C: Nonintervention | 58 | 4/54 | 13.1, >10 | NA | ①② |
| T: Schroth | 163 | 15/148 | 12.6, >10 | NA | |||||
| Büyükturan et al. (2024) | RCT | Turkiye | adolescents | T1: Schroth | 15 | 12/3 | 14.0 ± 1.9 | 24 | ①②③ |
| T2: Lyon | 16 | 12/4 | 14.2 ± 2.0 | 24 | |||||
| Zapata et al. (2023) | RCT | America | adolescents | C: Nonintervention | 22 | 15/7 | 12.5 ± 1.4 | 48 | ① |
| T: Schroth | 35 | 26/9 | 11.6 ± 1.1 | 48 | |||||
| Shen et al. (2023) | RCT | China | adolescents | T1: Schroth | 29 | NA | 13.75 ± 1.02 | 6 | ①②③ |
| T2: Schroth + Balance | 30 | NA | 13.47 ± 1.01 | 6 | |||||
| Qi et al. (2022) | RCT | China | adolescents | C: Nonintervention | 20 | 0/20 | 13.61 ± 1.33 | 12 | ① |
| T: Core | 18 | 0/18 | 13.94 ± 1.30 | 12 | |||||
| El et al. (2022) | RCT | Egypt | adolescents | C: Standard of care | 15 | 5/10 | 12.03 ± 1.94 | 12 | ①③ |
| T: Core | 15 | 6/9 | 11.5 ± 1.58 | 12 | |||||
| Won, Oh & Shen (2021) | RCT | Korea | adolescents | C: Standard of care | 10 | 0/10 | 15.90 ± 2.69 | 24 | ① |
| T: Core | 10 | 0/10 | 14.50 ± 2.50 | 24 | |||||
| Mohamed & Yousef (2021) | RCT | Egypt | adolescents | T1: Schroth | 17 | 0/17 | 14.50 ± 1.20 | 24 | ①② |
| T2: PNF | 17 | 0/17 | 14.90 ± 1.40 | 24 | |||||
| Kocaman et al. (2021) | RCT | Turkey | adolescents | T1: Schroth | 14 | 4/10 | 14.07 ± 2.37 | 10 | ①② |
| T2: Core | 14 | 3/11 | 14.21 ± 2.19 | 10 | |||||
| Gao et al. (2021) | RCT | China | adolescents | C: Nonintervention | 21 | 4/17 | 15.8 ± 1.5 | NA | ① |
| T: Schroth | 43 | 7/36 | 15.1 ± 1.6 | NA | |||||
| Abdel-aziem et al. (2021) | RCT | Saudi Arabia | adolescents | T1: Schroth | 25 | 7/18 | 15.04 ± 1.81 | 10 | ①② |
| T2: Schroth + Hippotherapy | 27 | 8/19 | 14.74 ± 1.79 | 10 | |||||
| Zapata, Sucato & Jo (2019) | RCT | America | adolescents | C: Nonintervention | 14 | 0/14 | 11.8 ± 0.9 | 48 | ① |
| T: BSPTS | 19 | 7/12 | 12.5 ± 1.5 | 48 | |||||
| Yu, Yang & Park (2019) | RCT | Korea | adolescents | C: Standard of care | 10 | 5/5 | 14.80 ± 2.90 | 8 | ① |
| T: Sling | 10 | 5/5 | 15.90 ± 2.69 | 8 | |||||
| Yagci & Yakut (2019) | RCT | Turkey | adolescents | T1: SEAS | 15 | 0/15 | 14.2 ± 1.5 | 16 | ①②③ |
| T2: Core | 15 | 0/15 | 14.0 ± 1.3 | 16 | |||||
| Negrini et al. (2019) | RCT | Italy | adolescents | C: Nonintervention | 53 | 13/40 | 12.03 ± 1.03 | 48 | ①② |
| T: SEAS | 145 | 41/103 | 12.07 ± 1.05 | 48 | |||||
| Schreiber et al. (2019) | RCT | Canada | adolescents | C: Standard of care | 25 | 1/24 | 13.3 ± 0.3 | 24 | ① |
| T: Schroth | 25 | 2/23 | 13.5 ± 0.375 | 24 | |||||
| Ko & Kang (2017) | RCT | Korea | adolescents | C: Nonintervention | 15 | NA | 12.80 ± 0.86 | 12 | ① |
| T: Core | 14 | NA | 12.71 ± 0.72 | 12 | |||||
| Kuru et al. (2016) | RCT | Turkey | adolescents | C: Nonintervention | 15 | 2/13 | 12.8 ± 1.2 | 24 | ①②③ |
| T: Schroth | 15 | 1/14 | 12.9 ± 1.4 | 24 | |||||
| Kim & HwangBo (2016) | RCT | Korea | adolescents | T1: Schroth | 12 | 0/12 | 15.60 ± 1.1 | 12 | ① |
| T2: Pilates | 12 | 0/12 | 15.3 ± 0.8 | 12 | |||||
| Monticone et al. (2014) | RCT | Italy | adolescents | C: Standard of care | 55 | 14/41 | 12.4 ± 1.1 | NA | ①②③ |
| T: SEAS | 55 | 16/39 | 12.5 ± 1.1 | NA |
Notes:
- NA
-
not reported
- RCT
-
randomized controlled trial
- C
-
Control group
- T
-
Experimental group
- ①
-
Cobb Angle
- ②
-
ATR
- ③
-
SRS-22
- PNF
-
Proprioceptive Neuromuscular Facilitation techniques
- Pilates
-
Pilates exercise
- Schroth
-
Schroth therapy
- BSPTS
-
BSPTS therapy
- SEAS
-
SEAS therapy
- Lyon
-
Lyon therapy
- Schroth + Sling
-
Schroth therapy + Sling training
- Schroth + Balance
-
Schroth therapy + Balance training
- Schroth + Hippotherapy
-
Schroth therapy + Hippotherapy
- Schroth + Core
-
Schroth therapy + Core stability training
- Core
-
Core stability training
- Sling
-
Sling training
Risk of bias in the studies
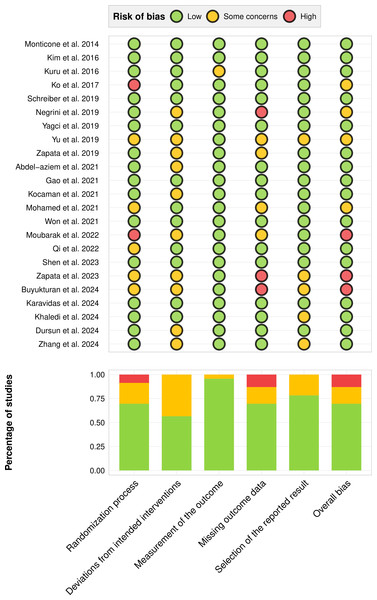
In the 23 studies included in the analysis, three studies (13%) had high overall bias, four studies (17.4%) had moderate or unclear overall bias, and 16 studies (69.6%) had low overall bias. See Fig. 2.
Figure 2: Risk of bias graph.
Note: Monticone et al., 2014; Kim & HwangBo, 2016; Kuru et al., 2016; Ko & Kang, 2017; Schreiber et al., 2019; Negrini et al., 2019; Yagci & Yakut, 2019; Yu, Yang & Park, 2019; Zapata, Sucato & Jo, 2019; Abdel-aziem et al., 2021; Gao et al., 2021; Kocaman et al., 2021; Mohamed & Yousef, 2021; Won, Oh & Shen, 2021; El et al., 2022; Qi et al., 2022; Shen et al., 2023; Zapata et al., 2023; Büyükturan et al., 2024; Karavidas et al., 2024; Khaledi et al., 2024; Manzak Dursun et al., 2024; Zhang et al., 2024.Network meta-analysis
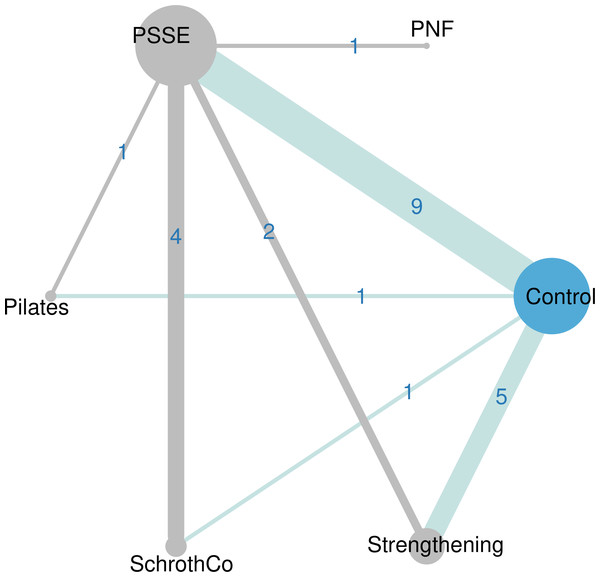
Figure 3 presents a comprehensive overview of the direct comparisons among the diverse therapeutic interventions aimed at addressing Cobb angle. Three outcome measures—Cobb angle, ATR, and SRS-22—constitute closed loops. In the context of Cobb angle assessment, three distinct closed loops are established: Control, PSSE, and SchrothCo; Control, PSSE, and Pilates; Control, PSSE, and Strengthening. A closed-loop in the ATR metric is formed: Control, PSSE, and SchrothCo. Two closed-loops are formed in the SRS-22 metric: Control, PSSE, and SchrothC, as well as Control, PSSE, and Core. Comprehensive insights pertaining to ATR and SRS-22 are available in the Supplemental Information.
Figure 3: Network plot for Cobb.
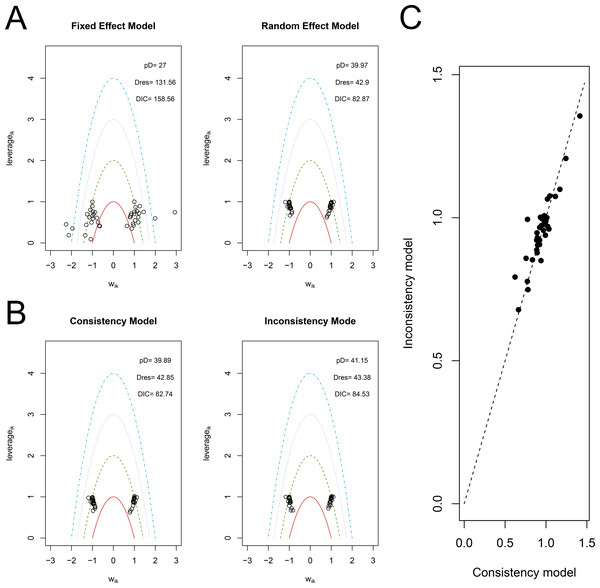
PSSE, PSSE modality: Physiotherapeutic Scoliosis-Specific Exercise; Strengthening, Strengthening training; SchrothCo, Schroth Combo modality: Schroth combined with other therapies; PNF, Proprioceptive Neuromuscular Facilitation techniques; Pilates, Pilates exercise.Figure 4 presents an analysis of the model fitting, displaying the assessment of the fit for both the fixed effects model and the random effects model in relation to the Cobb angle. The leverage plot presents the number of effective parameters, the residual deviations, and the DIC, which are valuable for guiding the model selection process. Figure 4A illustrates that the random effects model demonstrates a reduced DIC and a smaller number of outliers; thus, the findings regarding the Cobb angle suggest a favoring of the random effects model, a conclusion that similarly extends to ATR and SRS-22. Considering that consistency represents a fundamental assumption of NMA, we evaluated inconsistency by employing a random effects inconsistency model and juxtaposed it with our random effects consistency model, as illustrated in Fig. 4B. Upon assessing the compatibility of both models, we observed that the consistency model exhibited a marginally lower DIC for Cobb, ATR, and SRS-22, suggesting a commendable degree of consistency. Moreover, we constructed a plot. The findings for Cobb and ATR demonstrate a notable alignment between the two models, with the majority of leverage values approximating zero, while the outcomes for SRS-22 reveal a subtle tendency towards dispersion.
Figure 4: Model fitting diagram.
(A) The fixed and random-effect models for Cobb angle utilize plots and Deviance Information Criterion (DIC). DIC, Deviance Information Criterion; Dres, Deviance Residuals; pD, Posterior Mean Deviance; Wik, Adjustments for Study and Group Normal Distributions. (B) Leverage plots and DIC for Cobb’s consistency and inconsistency models. (C) Posterior mean deviance plots for Cobb’s consistency versus inconsistency models. DIC, Deviance Information Criterion; Dres, Deviance Residuals; pD, Posterior Mean Deviance; Wik, Adjustments for Study and Group Normal Distributions.The league table offers an extensive overview of the NMA results, emphasizing the importance of each intervention relative to the control group and alternative treatments. For the Cobb angle (Table 2), both SchrothCo (MD = −4.79, 95% CI [−8.56 to −1.11]) and PSSE (MD = −3.111, 95% CI [−5.27 to −0.9]) show significant differences compared to the control group. Regarding ATR, SchrothCo (MD = −3.03, 95% CI [−4.68 to −1.46]) and PSSE (MD = −2.37, 95% CI [−3.59 to −1.14]) also demonstrate significant differences relative to the control group. Furthermore, SchrothCo (MD = −3.2, 95% CI [−5.64 to −0.48]) and PSSE (MD = −2.54, 95% CI [−4.62 to −0.13]) significantly outperform core stability training, as well as SchrothCo (MD = −3.36, 95% CI [−6.26 to −0.61]) and PSSE (MD = −2.7, 95% CI [−5.2 to −0.19]) showing significant superiority over PNF. For the SRS-22 score, both SchrothCo (MD = 0.66, 95% CI [0.39–0.94]) and PSSE (MD = 0.44, 95% CI [0.22–0.66]) indicate significant differences when compared to the control group. Additionally, SchrothCo (MD = 0.45, 95% CI [0.04–0.70]) also shows a significant advantage over core stability training.
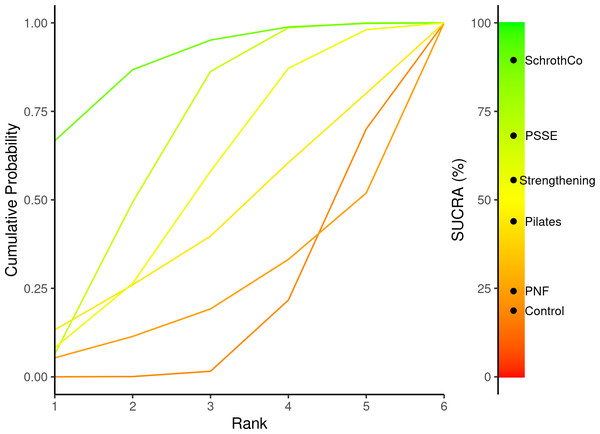
In our examination of the efficacy rankings of various exercise therapies, we undertook a probability ranking analysis, scrutinizing the posterior probabilities associated with each treatment’s ranking. This approach not only considers the probability of each therapy’s ranking but also offers a visual depiction through the cumulative ranking curve (SUCRA) plot, enabling an intuitive observation of the percentage probability rankings for each therapy. For the Cobb angle, the SUCRA plot analysis (Fig. 5) reveals the following SUCRA rankings: SchrothCo (89.46%) > PSSE (68.13%) > Strengthening (55.59%) > Pilates (43.92%) > PNF (24.22%) > Control (18.68%). For ATR, the SUCRA rankings are: SchrothCo (94.86%) > PSSE (77.52%) > Pilates (36.03%) > Control (34.44%) > Core (30.48%) > PNF (26.67%). Regarding the SRS-22 score, the rankings are as follows: SchrothCo (98.78%) > PSSE (64.67%) > Core (35.46%) > Control (1.09%).
Secondary analysis
The findings from the preceding phase of this study demonstrated that the SchrothCo and PSSE modalities are effective in addressing adolescent idiopathic scoliosis. Consequently, we undertook a secondary analysis to ascertain which treatment method demonstrates the highest efficacy.
Table 3 presents the results for the Cobb angle. Statistically significant differences were observed in comparison to the control group only in the PSSE modality with Schroth therapy (MD = −2.3, 95% CI [−5.45 to −0.66]). In the SchrothCo modality, significant efficacy was demonstrated by Schroth + Core (MD = −6.4, 95% CI [−13.63 to −0.89]) and by Schroth + Hippotherapy (MD = −5.27, 95% CI = -14.15 to −3.5). For the ATR, similarly, statistically significant differences were only observed in the PSSE modality with the Schroth therapy (MD = −2.79, 95% CI [−6.4 to −0.1]). In the SchrothCo modality, various combined interventions showed significant differences. Specifically, Schroth + Core (MD = −4.03, 95% CI [−9.37 to −0.98]), Schroth + Sling (MD = −3.12, 95% CI [−10.055 to −2.94]), and Schroth + Hippotherapy (MD = −3.39, 95% CI [−10.29 to −2.84]) exhibited significant efficacy. For the SRS-22, statistically significant differences were also only observed in the PSSE modality with the Schroth therapy (MD = 0.48, 95% CI [0.02–0.9]). In the SchrothCo modality, only Schroth + Core (MD = 0.79, 95% CI [0.13–1.43]) demonstrated significant efficacy.
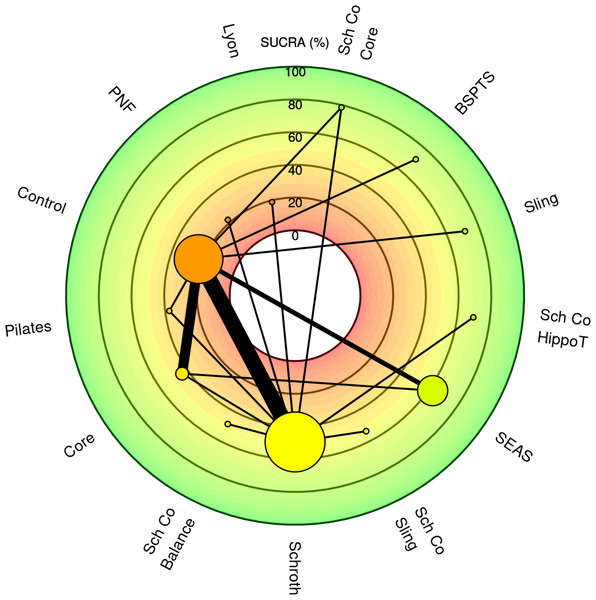
Figure 6 presents the radial SUCRA plot for a secondary meta-analysis concerning the Cobb angle. The top three SUCRA rankings for Cobb angle are as follows: Schroth + Core (78.57%) > BSPTS (71.37%) > Sling training (71.12%). For ATR, the top three SUCRA rankings are: Schroth + Core (79.08%) > Schroth + Hippotherapy (71%) > Schroth + Sling (67.92%). For SRS-22, the top three SUCRA rankings are: Schroth + Core (83.65%) > Schroth + Balance (71.01%) > Schroth + Sling (69.36%).
Covariate analysis affecting the pooling of main effects
The results of the regression analysis for potential covariates influencing the main effect are shown in Table 4. For the Cobb angle, the regression coefficient of the PSSE modality with the covariate (age) was β = −8.9921, 95% CI [−17.354 to −0.07019], indicating that PSSE had a more significant effect in reducing the Cobb angle in younger AIS patients. Additionally, for ATR, the regression coefficient of all treatment methods with the covariate (baseline Cobb angle) was β = −4.2393, 95% CI [−7.6124 to −0.8896], suggesting that all treatments were more effective in improving ATR in AIS patients with a smaller Cobb angle. Furthermore, no other significant moderating factors were identified.
| Control | Pilates | PNF | PSSE | SchrothCo | Strengthening | |
|---|---|---|---|---|---|---|
| Control | Control | −1.45 (−7.59, 4.6) | 0.44 (−6.55, 7.36) | −3.11 (−5.27, −0.97) | −4.79 (−8.56, −1.11) | −2.32 (−5.23, 0.53) |
| Pilates | 1.45 (−4.6, 7.59) | Pilates | 1.85 (−7.03, 10.86) | −1.68 (−7.65, 4.41) | −3.35 (−10.18, 3.47) | −0.89 (−7.49, 5.77) |
| PNF | −0.44 (−7.36, 6.55) | −1.85 (−10.86, 7.03) | PNF | −3.55 (−10.17, 3.02) | −5.21 (−12.68, 2.07) | −2.76 (−10.15, 4.64) |
| PSSE | 3.11 (0.97, 5.27) | 1.68 (−4.41, 7.65) | 3.55 (−3.02, 10.17) | PSSE | −1.68 (−4.98, 1.56) | 0.79 (−2.53, 4.08) |
| SchrothCo | 4.79 (1.11, 8.56) | 3.35 (−3.47, 10.18) | 5.21 (−2.07, 12.68) | 1.68 (−1.56, 4.98) | SchrothCo | 2.47 (−2.04, 7.03) |
| Strengthening | 2.32 (−0.53, 5.23) | 0.89 (−5.77, 7.49) | 2.76 (−4.64, 10.15) | −0.79 (−4.08, 2.53) | −2.47 (−7.03, 2.04) | Strengthening |
Notes:
- PSSE
-
PSSE modality: Physiotherapeutic Scoliosis-Specific Exercise
- Strengthening
-
Strengthening training
- SchrothCo
-
Schroth Combo modality Schroth combined with other therapies
- PNF
-
Proprioceptive Neuromuscular Facilitation techniques
- Pilates
-
Pilates exercise
Figure 5: SUCRA plot of Cobb angle.
PSSE, PSSE modality: Physiotherapeutic Scoliosis-Specific Exercise; Strengthening, Strengthening training; SchrothCo, Schroth Combo modality: Schroth combined with other therapies; PNF, Proprioceptive Neuromuscular Facilitation techniques; Pilates, Pilates exercise. Schroth, Schroth therapy.| BSPTS | Control | Core | Lyon | Pilates | PNF | Schroth + Balance | Schroth + Core | Schroth + Hippotherapy | Schroth + Sling | Schroth | SEAS | Sling | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BSPTS | BSPTS | 5.6 (−3.01, 14.23) | 3.77 (−5.61, 13.04) | 7.38 (−4.74, 19.17) | 4.59 (−6.53, 15.56) | 6.83 (−5.14, 18.69) | 3.26 (−8.54, 14.99) | −0.82 (−12.04, 10.57) | 0.34 (−12.03, 12.67) | 2.68 (−9.25, 14.36) | 3.28 (−5.93, 12.37) | 1.82 (−8.05, 11.69) | −0.07 (−12.46, 12.54) |
| Control | −5.6 (−14.23, 3.01) | Control | −1.84 (−5.4, 1.66) | 1.78 (−6.58, 10.04) | −1.02 (−7.92, 5.76) | 1.25 (−7.13, 9.41) | −2.32 (−10.43, 5.63) | −6.4 (−13.63, −0.89) | −5.27 (−14.15, −3.5) | −2.92 (−11.12, 5.02) | −2.3 (−5.45, −0.66) | −3.8 (−8.53, 1.13) | −5.62 (−14.65, 3.43) |
| Core | −3.77 (−13.04, 5.61) | 1.84 (−1.66, 5.4) | Core | 3.61 (−5.25, 12.42) | 0.83 (−6.77, 8.38) | 3.08 (−5.77, 11.75) | −0.51 (−9.1, 8.05) | −4.58 (−12.51, 3.52) | −3.42 (−12.78, 5.93) | −1.1 (−9.74, 7.42) | −0.48 (−4.79, 3.77) | −1.96 (−7.43, 3.76) | −3.79 (−13.4, 5.9) |
| Lyon | −7.38 (−19.17, 4.74) | −1.78 (−10.04, 6.58) | −3.61 (−12.42, 5.25) | Lyon | −2.77 (−13.07, 7.46) | −0.51 (−11.51, 10.35) | −4.1 (−14.8, 6.64) | −8.21 (−18.77, 2.63) | −7.01 (−18.49, 4.33) | −4.71 (−15.45, 5.93) | −4.08 (−11.83, 3.6) | −5.58 (−14.97, 4.17) | −7.4 (−19.52, 5.02) |
| Pilates | −4.59 (−15.56, 6.53) | 1.02 (−5.76, 7.92) | −0.83 (−8.38, 6.77) | 2.77 (−7.46, 13.07) | Pilates | 2.28 (−7.99, 12.49) | −1.3 (−11.36, 8.73) | −5.4 (−14.97, 4.56) | −4.26 (−14.82, 6.55) | −1.94 (−12.03, 8.15) | −1.31 (−8.04, 5.48) | −2.79 (−10.95, 5.72) | −4.63 (−15.8, 6.89) |
| PNF | −6.83 (−18.69, 5.14) | −1.25 (−9.41, 7.13) | −3.08 (−11.75, 5.77) | 0.51 (−10.35, 11.51) | −2.28 (−12.49, 7.99) | PNF | −3.58 (−14.28, 7.14) | −7.67 (−18.16, 3.17) | −6.53 (−17.79, 4.77) | −4.22 (−14.83, 6.62) | −3.54 (−11.25, 4.15) | −5.06 (−14.41, 4.7) | −6.88 (−18.98, 5.47) |
| Schroth + Balance | −3.26 (−14.99, 8.54) | 2.32 (−5.63, 10.43) | 0.51 (−8.05, 9.1) | 4.1 (−6.64, 14.8) | 1.3 (−8.73, 11.36) | 3.58 (−7.14, 14.28) | Schroth + Balance | −4.08 (−14.43, 6.49) | −2.93 (−14.04, 8.2) | −0.6 (−11.25, 9.84) | 0.02 (−7.46, 7.4) | −1.47 (−10.65, 8.07) | −3.33 (−15.17, 8.82) |
| Schroth + Core | 0.82 (−10.57, 12.04) | 6.4 (0.89, 13.63) | 4.58 (−3.52, 12.51) | 8.21 (−2.63, 18.77) | 5.4 (−4.56, 14.97) | 7.67 (−3.17, 18.16) | 4.08 (−6.49, 14.43) | Schroth + Core | 1.14 (−10.19, 12.16) | 3.51 (−7.18, 13.73) | 4.11 (−3.42, 11.37) | 2.63 (−6.04, 11.29) | 0.77 (−10.78, 12.37) |
| Schroth + Hippotherapy | −0.34 (−12.67, 12.03) | 5.27 (3.5, 14.15) | 3.42 (−5.93, 12.78) | 7.01 (−4.33, 18.49) | 4.26 (−6.55, 14.82) | 6.53 (−4.77, 17.79) | 2.93 (−8.2, 14.04) | −1.14 (−12.16, 10.19) | Schroth + Hippotherapy | 2.29 (−8.72, 13.44) | 2.93 (−5.39, 11.25) | 1.47 (−8.51, 11.65) | −0.4 (−12.83, 12.36) |
| Schroth + Sling | −2.68 (−14.36, 9.25) | 2.92 (−5.02, 11.12) | 1.1 (−7.42, 9.74) | 4.71 (−5.93, 15.45) | 1.94 (−8.15, 12.03) | 4.22 (−6.62, 14.83) | 0.6 (−9.84, 11.25) | −3.51 (−13.73, 7.18) | −2.29 (−13.44, 8.72) | Schroth + Sling | 0.62 (−6.82, 8.11) | −0.87 (−9.99, 8.66) | −2.71 (−14.5, 9.45) |
| Schroth | −3.28 (−12.37, 5.93) | 2.3 (0.66, 5.45) | 0.48 (−3.77, 4.79) | 4.08 (−3.6, 11.83) | 1.31 (−5.48, 8.04) | 3.54 (−4.15, 11.25) | −0.02 (−7.4, 7.46) | −4.11 (−11.37, 3.42) | −2.93 (−11.25, 5.39) | −0.62 (−8.11, 6.82) | Schroth | −1.49 (−6.99, 4.33) | −3.32 (−12.74, 6.34) |
| SEAS | −1.82 (−11.69, 8.05) | 3.8 (−1.13, 8.53) | 1.96 (−3.76, 7.43) | 5.58 (−4.17, 14.97) | 2.79 (−5.72, 10.95) | 5.06 (−4.7, 14.41) | 1.47 (−8.07, 10.65) | −2.63 (−11.29, 6.04) | −1.47 (−11.65, 8.51) | 0.87 (−8.66, 9.99) | 1.49 (−4.33, 6.99) | SEAS | −1.83 (−12.12, 8.27) |
| Sling | 0.07 (−12.54, 12.46) | 5.62 (−3.43, 14.65) | 3.79 (−5.9, 13.4) | 7.4 (−5.02, 19.52) | 4.63 (−6.89, 15.8) | 6.88 (−5.47, 18.98) | 3.33 (−8.82, 15.17) | −0.77 (−12.37, 10.78) | 0.4 (−12.36, 12.83) | 2.71 (−9.45, 14.5) | 3.32 (−6.34, 12.74) | 1.83 (−8.27, 12.12) | Sling |
Notes:
- PNF
-
Proprioceptive Neuromuscular Facilitation techniques
- Pilates
-
Pilates exercise
- Schroth
-
Schroth therapy
- BSPTS
-
BSPTS therapy
- SEAS
-
SEAS therapy
- Lyon
-
Lyon therapy
- Schroth + Sling
-
Schroth therapy + Sling training
- Schroth + Balance
-
Schroth therapy + Balance training
- Schroth + Hippotherapy
-
Schroth therapy + Hippotherapy
- Schroth + Core
-
Schroth therapy + Core stability training
- Core
-
Core stability training
- Sling
-
Sling training
Figure 6: Radial SUCRA plot for a secondary meta-analysis concerning the Cobb angle.
PSSE, PSSE modality: Physiotherapeutic Scoliosis-Specific Exercise; Strengthening, Strengthening training; PNF, Proprioceptive Neuromuscular Facilitation techniques; Pilates, Pilates exercise; Schroth, Schroth therapy; BSPTS, BSPTS therapy; SEAS, SEAS therapy; Lyon, Lyon therapy; Sch Co Sling, Schroth therapy + Sling training; Sch Co Balance, Schroth therapy + Balance training; Sch Co Hippo T, Schroth therapy + Hippotherapy; Sch Co Core, Schroth therapy + Core stability training; Core, Core stability training; Sling, Sling training.| Outcome index | Cobb | ATR | SRS-22 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Covariate | Treatment | β | 95% CI | β | 95% CI | β | 95% CI | ||
| Age (Continuous) | All | −2.0891 | −5.285, 1.0487 | −0.48915 | −2.5269, 1.465 | 0.1517 | −0.217259, 0.5098 | ||
| PSSE | −1.6688 | −5.708, 2.34293 | −0.2665 | −2.787, 2.0583 | 0.002008 | −0.420253, 0.4165 | |||
| Pilates | 2.9667 | −32.095, 48.58473 | 2.5737 | −39.055, 63.1352 | 0.421453 | −0.331777, 1.1422 | |||
| PNF | −1.323 | −61.743, 46.02285 | 4.3272 | −19.844, 45.5416 | 0.129176 | −0.396863, 0.6563 | |||
| SchrothCo | −3.1242 | −10.114, 3.68624 | −1.1375 | −4.471, 2.1640 | |||||
| Strengthening (Core) | −1.5971 | −7.141, 3.80076 | 1.9972 | −21.804, 32.1115 | |||||
| BMI (Continuous) | All | −1.38 | −5.126, 2.5144 | −1.5676 | −3.59674, 1.3078 | −0.3276 | −0.869305, 0.2390 | ||
| PSSE | −8.9921 | −17.354, −0.07019 | −1.1394 | −3.60449, 2.2895 | 0.02702 | −0.846134, 0.8906 | |||
| Pilates | 5.4887 | −14.680, 35.68850 | −0.4346 | −55.54185, 50.3324 | −0.31178 | −0.835091, 0.2054 | |||
| PNF | 6.6633 | −58.343, 127.01923 | −1.1182 | −53.56581, 44.4650 | 0.14482 | −0.897587, 1.1985 | |||
| SchrothCo | −5.872 | −18.871, 6.23163 | −1.5290 | −4.86732, 3.1114 | |||||
| Strengthening (Core) | 0.292 | −3.434, 4.03257 | 0.4911 | −6.42120, 7.7308 | |||||
| Baseline Cobb angle (Continuous) | All | 0.698 | −3.262, 4.5658 | −4.2393 | −7.6124, −0.8896 | −0.004166 | −0.457655, 0.4418 | ||
| PSSE | 2.0275 | −2.343, 6.2965 | −3.4950 | −6.9457, 0.06774 | −0.10557 | −0.538595, 0.3228 | |||
| Pilates | −3.0306 | −12.661, 5.8127 | −7.6305 | −98.1157, 36.46548 | 0.37247 | −0.278091, 1.0350 | |||
| PNF | −0.9561 | −219.855, 182.7906 | −3.5204 | −67.5764, 47.42337 | 0.47662 | −4.456943, 9.5030 | |||
| SchrothCo | −1.1105 | −17.430, 13.9504 | −2.5731 | −8.2437, 3.62849 | |||||
| Strengthening (Core) | −0.8052 | −8.347, 6.7985 | −4.0406 | −10.4965, 2.17772 | |||||
| Risser scores (Continuous) | All | 1.3705 | −2.7887, 5.2258 | 1.6301 | −8.26049, 8.731 | −0.07809 | −0.552109, 0.3936 | ||
| PSSE | 1.3318 | −2.8956, 5.3730 | 1.8465 | −5.6034, 8.994 | −0.138 | −0.593449, 0.3096 | |||
| Pilates | −2.9117 | −74.7083, 69.3258 | −1.3543 | −73.4431, 64.015 | 0.30818 | −0.502287, 1.2585 | |||
| PNF | 1.627 | −38.1322, 61.0186 | 2.1760 | −24.9271, 47.472 | −0.04034 | −1.416056, 1.2919 | |||
| SchrothCo | 1.6326 | −22.7120, 31.8739 | 2.2512 | −8.8446, 15.750 | |||||
| Strengthening (Core) | 0.1731 | −10.5846, 10.7711 | −0.6387 | −11.9817, 10.359 | |||||
| Risser scores (≤2 or >2) (Binary) | All | 0.9291 | −5.1368, 6.9618 | 0.78823 | −19.22578 , 27.917 | −0.06561 | −0.616787, 0.4822 | ||
| PSSE | 1.13999 | −4.6844, 7.1817 | 0.8726 | −13.57130, 13.472 | −0.1629 | −0.711525, 0.3625 | |||
| Pilates | −5.0691 | −163.9443, 71.6261 | −4.9974 | −125.32019, 59.934 | 0.2098 | −0.425028, 0.9106 | |||
| PNF | −11.46403 | −176.9407, 40.4653 | 3.111 | −46.36515, 73.840 | −0.6852 | −10.039542, 1.9960 | |||
| SchrothCo | −5.13042 | −58.7643, 25.3487 | 0.7569 | −22.95326, 25.887 | |||||
| Strengthening (Core) | −0.06945 | −9.7050, 9.4895 | −0.5876 | −15.54146, 12.029 | |||||
| Brace wearing (None or Acceptance) (Binary) | All | 3.692 | −0.5323, 7.7815 | 1.90978 | −1.3316, 5.5262 | 0.2894 | −4.43702, 7.6294 | ||
| PSSE | 3.9841 | −0.3342, 8.083 | 2.0723 | −0.8656, 5.8768 | −0.18483 | −1.778911, 1.5762 | |||
| Pilates | −1.7189 | −11.5427, 7.481 | −1.3141 | −94.0536, 86.9695 | 0.2605 | −1.296149, 2.0705 | |||
| PNF | 1.8104 | −53.4548, 63.474 | −1.502 | −26.9289, 19.7230 | 0.06748 | −4.466737, 5.1691 | |||
| SchrothCo | 0.7446 | −35.9090, 46.111 | 2.7862 | −39.2663, 60.5892 | |||||
| Strengthening (Core) | 1.9609 | −6.9304, 11.335 | 0.3993 | −5.8799, 7.1385 | |||||
Notes:
- PSSE
-
PSSE modality: Physiotherapeutic Scoliosis-Specific Exercise
- Strengthening
-
Strengthening training
- SchrothCo
-
Schroth Combo modality: Schroth combined with other therapies
- PNF
-
Proprioceptive Neuromuscular Facilitation techniques
- Pilates
-
Pilates exercise
Heterogeneity and publication bias assessment
The I2 statistic was used along with Cochran’s Q test to assess heterogeneity among studies, complemented by funnel plots and Egger’s test to examine publication bias. For the Cobb angle, the I2 = 0%, with a heterogeneity test p-value = 0.9698, and Egger’s test p-value = 0.7039. For ATR, the I2 = 0.61%, with a heterogeneity test p-value = 0.4544, and Egger’s test p-value = 0.8898. For SRS-22, the I2 = 0%, with a heterogeneity test p-value = 0.9620, and Egger’s test p-value = 0.6884. In summary, the overall heterogeneity was low, and no publication bias was observed. The above statistical analysis results can be confirmed in the Supplemental Information.
Evidence level assessment results
The evidence grading assessment results based on the CINeMA framework for this study are presented in Table 5.
| Control group vs | Within study bias | Reporting bias | Imprecision | Heterogeneity | Incoherence | Condence rating | ||
|---|---|---|---|---|---|---|---|---|
| Cobb | ATR | SRS-22 | ||||||
| PSSE | □ | □ | □ | □ | △ | Moderate | Moderate | Low |
| Schroth | □ | □ | □ | □ | △ | Moderate | Moderate | Low |
| BSPTS | □ | □ | △ | □ | △ | Low | NA | NA |
| SEAS | ○ | □ | △ | △ | △ | Low | Low | Low |
| Lyon | ○ | ○ | △ | ○ | □ | Low | Low | NA |
| SchrothCo | □ | △ | △ | △ | △ | Moderate | Moderate | Low |
| Schroth + Sling | □ | △ | △ | △ | △ | Low | Low | Low |
| Schroth + Balance | □ | □ | △ | △ | △ | Low | Low | Low |
| Schroth + Hippotherapy | □ | □ | △ | △ | △ | Low | Low | NA |
| Schroth + Core | □ | △ | △ | △ | △ | Low | Low | Low |
| Pilates | □ | □ | △ | □ | △ | Low | Low | NA |
| Strength | □ | □ | △ | △ | △ | Low | Low | Low |
| Core | □ | □ | △ | △ | △ | Low | Low | Low |
| Sling | □ | □ | △ | △ | △ | Low | NA | NA |
| PNF | ○ | □ | △ | □ | □ | Low | Low | NA |
Notes:
- Circle
-
Major concerns or high
- Box
-
Some concerns or unclear
- Triangle
-
No concerns or low
- Cobb
-
Cobb angle
- ATR
-
Axial Trunk Rotation
- SRS-22
-
Scoliosis Research Society Questionnaire
- PSSE
-
PSSE modality: Physiotherapeutic Scoliosis-Specific Exercise
- Strength
-
Strengthening training
- SchrothCo
-
Schroth Combo modality: Schroth combined with other therapies
- PNF
-
Proprioceptive Neuromuscular Facilitation techniques
- Pilates
-
Pilates exercise
- Schroth
-
Schroth therapy
- BSPTS
-
BSPTS therapy
- SEAS
-
SEAS therapy
- Lyon
-
Lyon therapy
- Schroth + Sling
-
Schroth therapy + Sling training
- Schroth + Balance
-
Schroth therapy + Balance training
- Schroth + Hippotherapy
-
Schroth therapy + Hippotherapy
- Schroth + Core
-
Schroth therapy + Core stability training
- Core
-
Core stability training
- Sling
-
Sling training
Discussion
Summary of evidence
This study employed a Bayesian network meta-analysis to evaluate the effects of exercise therapy on the Cobb angle, ATR and SRS-22 scores in subjects with AIS, thereby confirming the remarkable efficacy of exercise-based interventions for AIS. Preliminary results indicate that both the PSSE modality and combined Schroth-based approaches significantly reduce the curvature angle in AIS patients while improving their quality of life. Further analysis revealed that, for the Cobb angle, only the Schroth method demonstrated significant efficacy under the PSSE modality. In the SchrothCo modality, both Schroth + Core and Schroth + Hippotherapy showed statistically significant improvements. Regarding ATR improvement, the Schroth method was the only intervention to show significant efficacy under the PSSE modality. However, in the SchrothCo modality, interventions such as Schroth + Sling, Schroth + Hippotherapy, and Schroth + Core all demonstrated significant differences, highlighting their superior effectiveness in reducing ATR. Additionally, only the Schroth method and Schroth + Core intervention significantly improved quality of life. Therefore, it is noteworthy that Schroth + Core yielded the best outcomes in reducing the Cobb angle and ATR while enhancing quality of life, warranting further exploration in clinical research and therapeutic practice. The following sections will provide an in-depth discussion of these findings.
Considering the principal findings from the meta-analysis, an examination of the effects of various therapies within the PSSE modality was conducted. The meta-analysis conducted by Ma et al. (2023a) demonstrated that the PSSE-specific exercise therapy system outperformed other non-surgical treatments in correcting the Cobb angle and improving patients’ quality of life, particularly in terms of pain management, body image perception, and psychological well-being. Furthermore, the study by Seleviciene et al. (2022) indicated that, within the PSSE modality, only the Schroth method significantly reduced ATR, making it a promising option for broader clinical application. These findings are consistent with the preliminary meta-analysis results presented in this study. However, the meta-analysis by Wang et al. (2024) revealed that, in addition to the Schroth method significantly improving both the Cobb angle and ATR, the SEAS method was ranked as the most effective intervention for reducing the Cobb angle. This result is evidently inconsistent with the preliminary meta-analysis findings of this study. The discrepancy could be attributed to various factors, including differences in model selection, the number and quality of included studies, and population heterogeneity. In comparison, the studies included in this research are of higher quality, with the consistency model demonstrating a superior degree of DIC fit and minimal I2 values in Cochran’s Q test, indicating a lower degree of local inconsistency. This strengthens the reliability and scientific validity of the evidence provided. In summary, this study concludes that, without considering combined interventions, the Schroth method within the PSSE modality remains the optimal choice for simultaneously improving the Cobb angle, ATR and quality of life in AIS.
In relation to the outcomes of the secondary meta-analysis, significant emphasis is placed on the effectiveness of the Schroth method in conjunction with core stability training for patients with AIS, which constitutes a fundamental discovery of this research. Kocaman et al. (2021) conducted a study in which 28 patients with adolescent idiopathic scoliosis were randomly allocated to either a Schroth training group or a core training group. Following a 10-week intervention, the findings indicated that the Schroth training method demonstrated superior efficacy in addressing scoliosis and associated concerns, whereas core stability training yielded notable improvements in enhancing peripheral muscle strength. This may be attributed to the fact that Schroth training, by employing targeted postures and breathing techniques, successfully rectified irregular spinal alignment and improved the coordination and functionality of the musculature surrounding the spine. Furthermore, the meta-analysis conducted by Peng et al. (2024) reinforces this conclusion, demonstrating that Schroth training, via a meticulously crafted regimen of exercises and breathing techniques, effectively contributes to spinal correction and the rectification of muscle strength disparities. Conversely, core stability training fortifies the strength and stability of the core muscle groups, progressively augmenting strength and recruitment, thus establishing a resilient support system. This enhances the overall posture and functional performance of patients, thereby mitigating the pain experienced by those with AIS (Yagci & Yakut, 2019). In conclusion, both Schroth training and core stability training possess distinct benefits, and their therapeutic mechanisms differ significantly, necessitating a more thorough investigation.
The results of the covariate analysis indicate that the baseline Cobb angle does not significantly moderate the effectiveness of specific exercises in reducing the Cobb angle in AIS patients, this finding is supported by the study conducted by Baumann et al. (2024a). The study also revealed that PSSE-specific exercises significantly reduce the Cobb angle in younger AIS patients, which partially contradicts the findings of Baumann et al. Their study suggested that age does not have a significant moderating effect, whereas skeletal maturity was identified as a predictive factor for the risk of progressive scoliotic deformity (Lenz et al., 2021). Early intervention with appropriate exercise therapies at a younger age could effectively prevent further progression of spinal curvature. Additionally, it was observed that AIS patients with smaller baseline Cobb angles experienced greater reductions in ATR across all exercise therapies. No existing studies have corroborated this finding; however, patients with smaller Cobb angles may have larger intervertebral spaces and better flexibility, making them more amenable to correction. Further research is urgently needed to validate and expand upon these findings.
Potential mechanism of action of Schroth combined with core stabilization training for AIS
Recent studies reveal that patients with AIS demonstrate irregularities in TGF-β signaling within the paraspinal muscles, characterized by increased fibrosis and fat degeneration on the concave side, which results in a strength imbalance across both sides of the spine (Newton Ede & Jones, 2016). Furthermore, an overabundance of pressure applied to one side hinders bone development, whereas a lack of pressure on the opposite side encourages it (Guilbert et al., 2019). This imbalance may lead to scoliosis over time. Consequently, regardless of whether asymmetric activation or weakness induces scoliosis, fortifying the back and paraspinal muscles on the concave side aids in equilibrating muscular tension (Park et al., 2021). Targeted workouts specifically fortify the muscles on the convex side to equilibrate total tension, in accordance with Schroth methodology and core stability training. The Schroth method combines sensorimotor training, postural adjustment, and corrective breathing techniques to realign natural posture and improve postural control (Tan et al., 2009). Through the activation of isometric muscles on the concave side and the application of rotation angular breathing (RAB), the thorax undergoes a process of reshaping (Berdishevsky et al., 2016). adjusting, this method facilitates organic growth in concave regions, permitting subtle rotation about the thoracic axis, thereby enhancing, and refining the contour and architecture of the thorax (Beyer et al., 2017). Active self-correction, a fundamental component of Schroth therapy, underscores the importance of patients proactively modifying spinal posture in various planes to alleviate pressure on areas of deformity (Schreiber et al., 2016). This procedure not only refines posture but also augments muscle control, leading to improved spinal alignment and stability. Core stability training enhances the strength of 29 muscle pairs, notably the paraspinal, abdominal, and gluteal muscles, thereby providing stabilization for the spine, pelvis, and kinetic chain (Akuthota et al., 2008). The paraspinal muscles can be classified into two distinct groups: local stabilizers, which enhance segmental stiffness to regulate translation, and global stabilizers, which manage the range of motion through force generation (Lee, 2023). Enhancing core stability training fosters an intricate coordination between local and global stabilizers, harmonizing paraspinal muscle tension, delivering stable support in curved segments, and mitigating excessive movement. At the level of neural signaling, the fortification of core muscles augments proprioceptive awareness regarding muscle contraction, thereby enhancing the efficiency of transmission between passive spinal structures and central regulatory mechanisms, which in turn sustains vertebral-pelvic stability (Chwala et al., 2014; Czaprowski et al., 2018; Xiao et al., 2021). Nonetheless, the efficacy of Schroth therapy remains inadequately substantiated in relation to neural signaling pathways (Baumann et al., 2024b), necessitating additional research to elucidate any potential overlaps with core training methodologies. In conclusion, the integration of Schroth with core stability training synthesizes diverse therapeutic methodologies, tackling AIS through a multifaceted lens—self-posture adjustment, breathing correction, structural support, neuromuscular control, and proprioceptive enhancement. This integrated approach meticulously addresses fundamental aspects of postural and functional rehabilitation, highlighting considerable therapeutic promise through a multifaceted synergy.
Limitation
Firstly, the limited number of studies included in certain subgroup analyses restricts the statistical power of the results, necessitating cautious interpretation when applying these findings. On the other hand, although this study’s covariate analysis examined factors such as brace-wearing, Risser staging, age, baseline Cobb angle, and body mass index (BMI), it was constrained by the limited reporting of key scoliosis subtypes, single-gender cohorts, and follow-up durations in the included literature. As a result, the covariate analysis lacks comprehensiveness, and the relatively small sample size may have reduced statistical power and increased the likelihood of Type II errors. Future research should focus more on investigating the efficacy of exercise interventions with and without brace-wearing, as well as the potential influence of Risser staging on treatment outcomes. Despite these limitations, this study represents the most comprehensive and highest-quality systematic review and meta-analysis conducted to date on this topic.
Conclusion
This article utilized a network meta-analysis to assess and contrast the therapeutic advantages of various exercise therapies for AIS, with the objective of offering evidence-based recommendations for exercise specialists, physical therapists, and clinicians. Recent findings suggest that the combination of Schroth therapy and core stability training yields the most significant reductions in the Cobb angle and axial trunk rotation, while also enhancing overall quality of life. Future endeavors necessitate comprehensive clinical randomized controlled trials and rigorous studies to further corroborate and reinforce these conclusions.